Kwashiorkor is a severe form of malnutrition known as protein-energy malnutrition or protein-calorie malnutrition that is caused mainly by an insufficient amount of protein needed by the body with the conservation of subcutaneous fat. Kwashiorkor is seen mostly in children of 1 to 3 years and affects mostly children in Africa, Latin America, and Asia.
Table of Contents
Causes of Kwashiorkor
- Malnutrition from lack of protein or low/inadequate protein diet: this could be as a result of inadequate feeding of child (the food may be available but feeding may not be adequate for the child).
- Infections such as measles, diarrheal diseases, intestinal parasites, Whooping cough, HIV/AIDS and malaria. These infections predispose the child to Kwashiorkor because they interfere with appetite, digestion of food, absorption and utilization of nutrients. Infections complicate Kwashiorkor and in turn, Kwashiorkor predisposes to infections.
- Free radicals exceeding the amount of antioxidants needed to defend the body
- Poverty and unemployment makes feeding difficult due to lack of money and hence, the cost of buying meat, egg or other protein containing food is high.
- Low birth weight infants are predisposed to malnutrition than normal infants.
- Lack of exclusive breastfeeding may be an important cause of Kwashiorkor even before 1 year due to predisposition of the child to recurrent diarrhea and infections
Kwashiorkor mostly occurs in children that have been weaned suddenly or when weaning begins with food that has inadequate dietary protein.

Signs and Symptoms of Kwashiorkor
- Growth retardation (failure to thrive)
- Edema (swelling of the body)
- Muscle wasting
- Apathy (loss of interest) and other mental changes such as irritability
- Skin changes such as dermatosis
- Hair changes such as thin and brownish/red hair
- Signs of micronutrient deficiency
- Intractable diarrhea
- Vomiting
- Loss of appetite (refusal to eat)
- Mucous membrane changes
- Moon face
- Hepatomegaly (enlargement of the liver due to fat deposition)
Poor growth
A child with Kwashiorkor will not grow well compared with other normal children of the same age because of the lack of protein needed for metabolism and growth and production of other proteins needed by the body such as hormones and antibodies.
Edema
The swelling normally starts from the feet and then spreads to the leg and other parts of the body. The swelling of the body may be due to the low amount of a protein in the blood known as albumin that is responsible for normalizing the movement of fluids between the blood vessels and the surrounding cells of the body. When albumin is low, more fluids move into the surrounding of the cells (extravascular space) making the body swell. Children with Kwashiorkor have abdominal swelling making them look as if they are pregnant.
Wasting of the muscles
The loss of appetite in Kwashiorkor could lead to low food intake and less energy will be available for use in the body. In trying to provide energy, the body starts to break down the muscles of the body for use as energy. This process is referred to as gluconeogenesis. This breakdown leads to diminishing the bulk of the muscles, making the child weak and unable to walk or stand, giving a false impression of paralysis.
Mental changes
Children with Kwashiorkor are usually irritable. Little things get them angry and may cry, they do not want to be touched or disturbed and they have no interest in whatever may seem interesting to other children. You will often find children with Kwashiorkor looking dull, unhappy, and very miserable.
Skin changes
There are skin changes in Kwashiorkor such as changes in skin color. The skin also becomes flaky and cracked
Hair changes
The hair changes in Kwashiorkor manifest with a change in color to brown or red and are easy to pluck.
Moon face
The swelling of the face and cheeks makes the child looks as if the face is like that of the moon.
Hepatomegaly
Accumulation of fats in the liver leads to an enlarged liver and this inhibits the normal function of the liver; hence, the low albumin in the blood leads to body swelling in Kwashiorkor.
Intractable diarrhoea
Kwashiorkor makes the intestines become atrophied (shrink) making it difficult for digestion of food to occur. This indigestion leads to the accumulation of food in the intestines that draws water from the body into the intestines causing diarrhea. There is also an inability to tolerate the type of sugar contained in milk known as Lactose; hence children with Kwashiorkor cannot take and should not be given milk containing lactose. They are said to be lactose intolerant.
Signs of deficiency of micronutrients
Micronutrients deficiencies are very common in Kwashiorkor and any type of deficiency could occur or a combination of the nutrients deficiency may occur. They may present with blindness in severe cases of vitamin A deficiency or may have anemia in iron deficiency. You can learn more about micronutrient deficiency.
Diagnosis of Kwashiorkor
According to the Modified Wellcomes classification of malnutrition, the diagnosis of Kwashiorkor is made when the weight for age is greater than 80% in a child with body swelling. When the weight for age is from 60 to 80% with body swelling, then the child is referred to as Underweight Kwashiorkor. When the weight-for-age is less than 60% with the presence of edema (body swelling), then the child has Marasmic Kwashiorkor. Weight for age refers to the weight of the child compared to the age in reference to the same weight of normal children of his/her age.
Laboratory investigations in Kwashiorkor
Laboratory tests are done in order to help diagnose the presence of other diseases and help in treatment. The tests do not show if the child has Kwashiorkor or not, as diagnosis of Kwashiorkor depends on clinical findings and examinations. The laboratory tests help in management (treatment) and include:
- Packed cell volume (PCV) to check for anemia
- Differential white blood cell count may show presence of infections
- Urinalysis and urine microscopy may show if there is urinary tract infection
- Stool microscopy to check for presence of gastrointestinal tract parasites
- Chest radiograph helps to rule out tuberculosis and may show any pulmonary complications
- Test for Human Immunodeficiency virus (HIV)
Features of Poor prognosis in Kwashiorkor
- Overwhelming sepsis
- Hypothermia
- Intractable seizure
- Altered sensorium
- Hypoglycemia
Marasmic Kwashiorkor
This is a combination of Kwashiorkor and Marasmus occurring together in a child and the signs and symptoms cannot be pinpointed to a single form of Protein-energy malnutrition.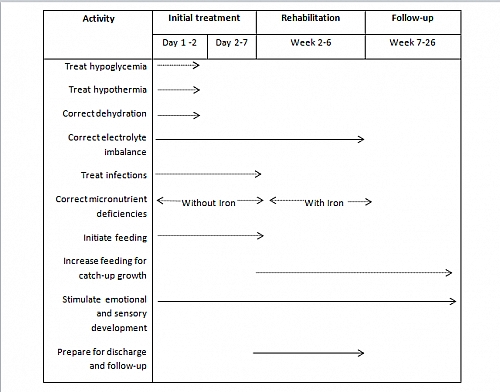
Timeline for the management of a child with severe malnutrition such as Kwashiorkor
Treatment of Kwashiorkor
Kwashiorkor treatment involves both medical treatment and dietary therapy. It is treated just like any other forms of severe protein-energy malnutrition. The treatment is done in 3 phases and involves timelines that should be followed correctly.
Treatment phases
- Stabilization phase: this is the initial treatment phase that is done within the first 7 days of admission and involves treating the conditions that may easily cause death (life threatening conditions) or complications
- Rehabilitation phase: this is started from the second week to the sixth week. It involves proper investigations to know the cause of the Kwashiorkor and appropriate treatment
- Follow up phase: this starts from week 6 to the 6th month. It involves serial weight measurements during visits to ensure appropriate weight gain.
STABILIZATION PHASE
This involves the correction of life-threatening conditions such as hypoglycemia, dehydration, and hypothermia on the 1st and 2nd day of admission.
Correction of hypoglycemia in Kwashiorkor
The low glucose level in the blood is a frequent cause of death and re-feeding of the child should be commenced and continued subsequently every 2- 3 hours. If feeding is not possible, then 50ml of 10% dextrose should be given orally or by use of a nasogastric tube (NG Tube). If the child is unconscious or critically ill, then intravenous glucose solution should be given.
Correction of Hypothermia
Children with Kwashiorkor cannot regulate their body temperature and this becomes worse in the mornings when the environmental temperature is very low. This can be corrected by wearing warm clothes and the mother can practice kangaroo mother care by holding the child such that her skin and that of the child comes in contact while being covered.
Persistent low body temperature even with the above methods may point to septic shock and other symptoms of shock should be assessed and treated appropriately of which plasma or blood transfusion may be required with antibiotics.
Correction of Dehydration
Accurately assessing the level of dehydration in severe forms of protein energy malnutrition can be difficult and is safer to assume there is some level of dehydration. Rehydration should be commenced immediately orally or by use of NG Tube except in cases where the patient is critically ill or unconscious, then intravenous rehydration can be used. Rehydration is corrected in Kwashiorkor and any other form of protein-energy malnutrition using a special Rehydration Solution for Malnutrition (ReSoMal) because of its low sodium content, the WHO ORS should be avoided.
For severely dehydrated patients or those who presented with septic shock, rehydration should be done with half-strength Darrows solution with 5% dextrose or Ringers lactate with 5% dextrose or 0.45% normal saline in 5% dextrose.
Correction of electrolytes disorders and mineral deficiencies
In Kwashiorkor, there is low potassium, magnesium, copper, and zinc in the blood. This can be treated using ReSoMal. Iron therapy should be started when infections have been treated.
Vitamin supplements can be given in the form of multivitamin preparations.
Treatment of infections
Common infections associated with Kwashiorkor include measles, malaria, skin infections, urinary tract infections, respiratory tract infections, and septicemia. These infections present atypically and may be difficult to diagnose clinically, hence broad-spectrum antibiotics should be used.
REHABILITATION PHASE
The rehabilitation phase requires continued treatment by taking a detailed medical history of the condition and appropriate examination to find the cause of the Kwashiorkor. It also involves treatment of any associated conditions such as anemia, xeropthalmia, congestive cardiac failure, and dermatosis.
The dermatosis (skin lesion) in Kwashiorkor can be treated by zinc supplements or topical application of 0.01% potassium permanganate. Castor oil or zinc ointment can be applied.
FOLLOW UP PHASE
Follow-up should be carried out to ensure appropriate weight gain by serial weight measurements.
Complications of Kwashiorkor
- Severe Infections such as Bronchopneumonia and gastrointestinal tract infections
- Electrolyte imbalances such as low calcium in blood (hypocalcaemia) and low phosphate (hypophosphatemia)
- Mental retardation: this occurs during periods of brain development.
- Growth retardation
- Blindness as a result of vitamin A deficiency.
- Heart failure: not common but may occur as a result of anemia or low potassium (hypokalemia)
- Low immunity
- Coma
- Death
Differential diagnosis
- Pellagra
- Scurvy
- Acrodermitis entropathica
- Dermatitis herpitiformis
Prevention
The World Health Organisation (WHO) provided a priority program known as GOBIF which stands for:
- Growth monitoring for easy detection of failure to thrive
- Oral rehydration therapy for treatment of diarrhea
- Exclusive Breastfeeding
- Immunization to prevent infections
- Family planning
Source:
- Paediatric and Child Health in a Tropical Region by Azubuike and Nkanginieme
- W.H.O: The World Health Report – “Choosing Interventions to Reduce Specific Risks“
- Images credits from Youtube Channel (Fabin Salgado) Video: https://www.youtube.com/watch?v=4j8qUkSjMsA on Kwashiorkor
