Birth asphyxia is a medical emergency condition thatoccurs as a result of oxygen lack which is called hypoxia. The lack of oxygen could be caused by lack of blood flow to the brain (known as ischemia) or insufficient oxygenation of blood in the lungs. This lack of oxygen causes different harmful effects on the body system of the baby such as metabolic acidosis and accumulation of carbon dioxide in the body. When left untreated or if not treated immediately, birth asphyxia leads to a serious conditioned known as Hypoxic ischemic encephalopathy (HIE). This condition is the severe form of birth asphyxia and prompt intervention is needed to prevent HIE from occurring in an asphyxiated baby.
Birth asphyxia is also called perinatal asphyxia because the asphyxia can occur even before a baby is born or when a baby is born or after a baby is born. Perinatal period refers to the period that surrounds birth (i.e. before, during and after birth) with a large number occurring antepartum (before birth) and intrapartum(during birth); hence birth asphyxia can be called perinatal asphyxia. It is also called Neonatal asphyxia because it occurs mostly in infants that are not more than 28 days of age. We may use any of the mentioned names for the purpose of description based on the context in this article. However, the American Academy of Pediatrics (AAP) and American College of Obstetrics and Gynecologists (ACOG) recommended using HIE due to the fact that this term correctly describes the severity and complication (encephalopathy) that is caused by the asphyxia. The AAP and ACOG also advised avoiding the use of perinatal asphyxia or birth asphyxia because they do not point the time that the injury to the brain occurred and the use of the terms do not show as to whether the brain was normal before the HIE developed or the baby was actually born with it. The terms therefore do not outline all the components of HIE.
Table of Contents
- Epidemiology of Birthasphyxia
- Causes of birth asphyxia and associated risk factors
- PATHOPHYSIOLOGY OF PERINATAL ASPHYXIA
- Classification of Birth(Perinatal) asphyxia using APGAR score
- Clinical signs and symptoms of Birth asphyxia
- Signs and symptoms of HIE (Hypoxic ischemic encephalopathy)
- CLINICAL STAGES OF PERINATAL HYPOXIC ISCHAEMIC BRAIN INJURY: SARNAT AND SARNAT STAGING
- MULTIORGAN SYSTEMIC EFFECTS OF BIRTH ASPHYXIA
- Differential diagnosis of birth asphyxia
- Investigations
- Treatment and Management of Birth asphyxia
- Predictors of Poor Neurodevelopmental outcome in Birth asphyxia
- Prevention of Birth asphyxia
- Complications and long term effects of birth asphyxia:
- Detection of infants at risk of perinatal asphyxia:
- Prognosis of birth asphyxia
Epidemiology of Birthasphyxia
Perinatal asphyxia contributes significantly to reduction of quality of life because of its complications and effects and can also cause death.
The World Health Organization (WHO) states that about 1 million children worldwide die from a diagnosis of birth asphyxia and about 1 million survivors living with the long term complications such as HIE or other neurological disabilities, especially in developing countries. The tendency of having birth asphyxia is the same across all races and both gender.
Causes of birth asphyxia and associated risk factors
There are certain medical conditions that increase the tendency of a baby having birth asphyxia. These conditions often occur in complicated pregnancy. They can be grouped as factors occurring before birth (antepartum factors), during birth (intra-partum factors) and after birth (post-partum factors).
Causes of birth asphyxia occurring before delivery
- Hypertensive disease of pregnancy like pre-eclampsia and eclampsia
- Severe maternal hypotension
- Abnormal uterine contractions causing fetal distress
- Congenital infections
- Intrauterine growth restriction (IUGR)
- Placental abruption cutting blood and oxygen supply to the fetus
- Fetal anaemia as in rhesus incompatibility
- Postmaturity leading to insufficient supply of oxygen and blood as a result of over demand.
Causes of birth asphyxia occurring during delivery
- Abnormal labor leading to trauma such as shoulder dystocia or breech presentation of fetus
- Cord prolapse
- Malpresentation and also Vasa praevia.
Causes of birth asphyxia occurring after delivery
- Inability of baby to cry immediately after birth in order to establish lung inflation
- Congenital heart diseases
- Severe circulatory insufficiency such as in severe blood loss or septic shock
- Persistent pulmonary hypertension of the newborn
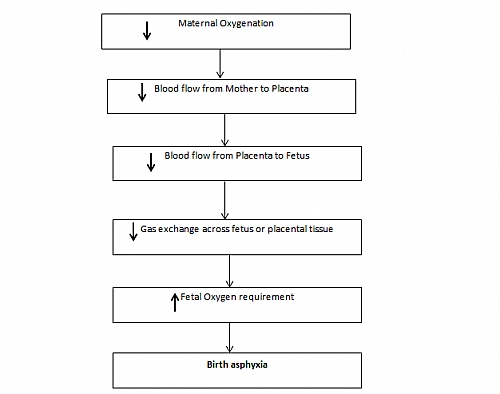
PATHOPHYSIOLOGY OF PERINATAL ASPHYXIA
For adequate lung function to occur at birth, there shouldnt be any abnormality that interferes with control of respiration, the fluid that fills lungs in the fetus should be removed and there should be a good oxygen/carbon dioxide exchange between the air sacs (alveoli) and the blood.
The babys first breath during vaginal delivery together with intermittent compression of the chest allows removal of fluid in the lung. There are various stimuli that are responsible for the babys first breath; these stimuli include a decline in partial pressure of oxygen (PO2), decreased PH and rise in partial pressure of carbon dioxide (PCO2) mainly due to: interruption of the placental circulation, redistribution of cardiac output after clamping of the umbilical cord, a fall in body temperature and tactile stimuli. The pressure required for inflating the babys lungs are high which makes it easier for term infants compared to low birth weight (LBW) infants who have a very compliant chest wall and may find it difficult to draw the first breath. Forced Residual Capacity (FRC) is least in most premature infants due to the presence of atelectasis. Also, the premature infants have abnormalities in the ventilation-perfusion ratio and also, LBW infants may have a low PaO2(50-60 mmHg) and an elevated PaCO2 as a result of atelectasis, intrapulmonary shunting and hypoventilation. The smallest immature infants have the most profound disturbances, which may resemble Respiratory Distress Syndrome (RDS).
With onset of respiration and lung expansion, pulmonary vascular resistance falls, followed by a gradual transition from fetal to adult circulation as the foramen ovale and ductus arteriosus close.
In the event that the transition from fetal to adult circulation fails to progress normally, the birth asphyxia occurs with accompanying complications. The fetal circulatory response to acute hypoxemia (decreased arterial partial pressure of oxygen, PO2) or asphyxia (decreased arterial PO2 and increased partial pressure of carbon dioxide, PCO2) has been well described in both experimental animals and humans.
In early stages of birth asphyxia, blood flow to the liver, kidneys, intestines, muscles and lungs decreases; while the blood flow to the vital organs such as the heart and brain and adrenal glands and to a lesser extent the placenta, increases. The blood flow through the umbilical vein is redistributed within the right atrium to favor perfusion of the heart and brain. The net effect of this is preservation of oxygen flow to the heart and brain at the expense of other organs to an extent that hypoxemia is severe enough to cause circulatory collapse.
The degree of organ damage following perinatal asphyxia is dependent on the oxygen requirement of the organ involved and the severity of the asphyxia; the brain is mostly affected with about 70% of infants with birth asphyxia showing signs of HIE.
Classification of Birth(Perinatal) asphyxia using APGAR score
- Severe birth asphyxia: with APGAR score of 0-3
- Moderate birth asphyxia with APGAR score of 4-6
- Mild depression with APGAR score of 7-10
Criteria for diagnosis of SEVERE perinatal asphyxia
- Profound hypoxemia or mixed acidemia with PH of <7 on umbilical cord arterial blood sample, if obtained.
- Persistence of an APGAR Score of 0-3 for more than 5 minutes
- Neurologic manifestation in the immediate neonatal period including seizure, hypotonia, coma or hypoxic ischemic encephalopathy (HIE).
- Evidence of multi-organ dysfunction in the immediate neonatal period
These criteria were defined by American Academy of Pediatrics (AAP) and American College of Obstetrics and Gynecologists (ACOG).
EARLY PHASE OF BIRTH ASPHYXIA
Primary Apnea
In this phase of birth asphyxia, there is transient increase in heart rate with associated fast breathing with increase in cardiac output and peripheral constriction of blood vessels that leads to hypertension as a result of the mild increase in blood and central venous pressure. Observation shows cyanosis with good circulation. This phase of birth asphyxia last for about 1 to 2 minutes
Events in prolonged birth asphyxia
Asphyxia leads to a decrease in Blood pressure and cardiac output thereby leading to decreased central blood flow and also lactic acidosis. Lactic acidosis occurs due to anaerobic metabolism from the low glucose level in the blood. Low glucose also leads to decrease in ATP which will cause cellular energy failure and also failure of the ion pumps leading to accumulation of sodium, chloride, calcium and water in the cells. The accumulation of these ions in the cells have negative effects: the increase in sodium leads to swelling of the cell, a condition referred to as cytotoxic edema while the accumulated calcium causes increased glutamate, free radicals (harmful to cells) and fatty acids/lipids which all disrupt the metabolism of the cell.
Secondary Apnea
When birth asphyxia becomes prolonged, then secondary apnea ensues with rapid gasps, low blood pressure (hypotension), severe bradycardia (slowing of the heart rate) and deterioration of the babys circulation. There is a redistribution of blood to the vital organs such as the heart, brain, adrenal gland and the kidneys, a conditioned referred to as the diving reflex. The central blood flow (CBF) may become pressure-passive causing the perfusion of the brain to depend on the systemic blood pressure; as the systemic blood pressure falls, the central blood flow falls below the critical level and hypoxia of the brain occurs. At the early phases of brain injury, there is release of neurotransmitter (GABA) and also a drop in temperature of the brain.
At the cellular level, the damage to the neurones is an evolving process and the magnitude of the damage is dependent on the following:
- The extent of the initial injury The nature, duration and severity of the primary injury are crucial in determining the extent of final damage. Following the initial phase of energy failure from the asphyxia injury, cerebral metabolism may recover, only to deteriorate in the second phase.
- Reperfusion injury is a second determinant of the extent of brain damage.
- By 6-24 hours after the initial injury, a new phase of neuronal destruction sets in that is characterized by apoptosis (i.e. programmed cell death); this is also known as delayed injury and the phase may continue for days to weeks. The severity of brain injury in this phase corresponds to the severity of the long term effects such as HIE in infants. The modern treatment interventions of birth asphyxia are geared towards reducing the neurological destruction that occurs during this phase.
Clinical signs and symptoms of Birth asphyxia
Signs and symptoms of hypoxic encephalopathy (HIE) at the time of birth due to asphyxia or brain hypoxia remote from the time of delivery.
The signs and symptoms of HIE are:
- Yet to cry since birth or poor and weak cry at birth
- Low Apgar score
- Convulsion or unconsciousness
- Weak or floppy
- Symptoms of multiple organ involvement
- Prolonged labor is a common cause, hence the mother may have a history of labor being prolonged.
- History of difficulties with delivery , particularly problems with delivering the after-coming head in breech presentation
Signs and symptoms of HIE (Hypoxic ischemic encephalopathy)
- Mild HIE (Hypoxic Ischemic Encephalopathy)
– Transient behavioral abnormalities, such as poor feeding, irritability or excessive crying or sleepiness may be observed in the baby.
– Muscle tone may be increased slightly and deep tendon reflexes may be brisk during the first few days. However, by 3-4 days of life, the CNS examination becomes normal - Moderately severe HIE
– The infant will be lethargic, with significant hypotonia and diminished deep tendon reflexes
– There are reduce or absent grasping, Moro, and sucking reflexes
– The intermittent periods of apnea
– Seizures occurring within the first 24 hours of life
– Full recovery within 1-2 weeks is possible and correlates with good prognosis in the long term
– There may be preceding period of well-being which may also be followed by sudden deterioration, suggestive of reperfusion injury; there may also be increase in intensity of seizure. - Severe HIE
– In severe HIE, stupor or coma is typical and infant may not respond to any physical stimulus
– There may be irregular breathing that will necessitate respiratory support therapy.
– Low tone with decreased deep tendon reflexes also occur in severe HIE
-Absent neonatal reflexes such as sucking, grasping, swallowing and Moro reflexes
– Examination of the cranial nerves reveals disturbances in ocular motion such as a skewed deviation of the eyes, nystagmus, bobbing, and loss of dolls eye.
– Pupils may be dilated, fixed or poorly reactive to light
– Seizures occur early and often and may be initially resistant to conventional treatment. The seizures are usually generalized seizures with increase in frequency, 2-3 days after onset corresponding with the phase of reperfusion injury. The seizures paradoxically subside as brain injury progresses and the Electroencephalogram (EEG) becomes isoelectric or shows a burst suppression pattern, at this time wakefulness may deteriorate further with cerebral edema as evidenced by bulging of the fontanelles.
– The irregularities of heart rate and Blood pressure occur commonly during the period of reperfusion injury and death from cardiorespiratory failure is also common.
CLINICAL STAGES OF PERINATAL HYPOXIC ISCHAEMIC BRAIN INJURY: SARNAT AND SARNAT STAGING
This staging system was proposed by Sarnat and Sarnat in 1976 and it is often used in diagnosing HIE. Stages I, II and III correlate with mild, moderate and severe hypoxic ischemic encephalopathy
| STAGE 1 | STAGE 2 | STAGE 3 | |
| Level of Consciousness | |||
| Hyperalert | Lethargy or obtunded | Stuporous | |
| Neuromuscular control | |||
| Muscle tone: | Normal | Mild hypotonia | Flaccid |
| Posture: | Mild distal flexion | Strong distal flexion | Intermittent decerebration |
| Stretch reflexes: | Overactive | Overactive | Decreased or absent |
| Segmental myoclonus: | Present | Present | Absent |
| Complex Reflexes | |||
| Sucking | Weak | Weak or absent | Absent |
| Moro | Strong, low threshold | Weak, incomplete, high threshold | absent |
| Oculovestibular | Normal | Overactive | Weak or absent |
| Tonic neck | Slight | Strong | Absent |
| Autonomic function | |||
| Generalized (sympathetic) | Generalized (parasympathetic) | Both systems depressed | |
| Pupils: | |||
| Mydriasis | Miosis | Variable, often unequal, poor light reflex | |
| Heart rate: | |||
| Tachycardia | Bradycardia | Variable | |
| Bronchial and salivary secretion: | |||
| Sparse | Profuse | Variable | |
| GI motility: | |||
| Normal or decreased | Increased, diarrhea | Variable | |
| Seizures: | |||
| None | Common: focal or multifocal | Uncommon (excluding decerebration) | |
| EEG Findings: | |||
| Normal (awake) | Early: low voltage continuous delta and theta. Late: periodic pattern (awake) Seizures: focal 1-1Hz spike and wave |
Early: periodic pattern with isopotential phases Late: totally isopotential |
|
| Duration: | |||
| 1-3 days | 2-4 days | Hours to weeks | |
MULTIORGAN SYSTEMIC EFFECTS OF BIRTH ASPHYXIA
- Central Nervous System (CNS): hypoxic ischemic encephalopathy, infarction, intracranial haemorrhage, seizures, cerebral edema, hypotonia and hypertonia.
- Cardiovascular System: Myocardial ischemia, poor contractility, cardiac stun, tricuspid insufficiency and hypotension.
- Pulmonary system: Pulmonary hypertension, pulmonary haemorrhage and respiratory distress syndrome.
- Renal system: Acute tubular or cortical necrosis
- Adrenal system: adrenal haemorrhage
- Gastrointestinal System: Gastrointestinal perforation, ulceration with hemorrhage, necrosis
- Metabolism: Inappropriate secretion of antidiuretic hormone, hyponatremia, hypoglycemia, hypocalcemia and myoglobinuria
- Integumentary System: Subcutaneous fat necrosis
- Hematological System: disseminated intravascular coagulation
Differential diagnosis of birth asphyxia
Other diseases that may mimic birth asphyxia include:
- Developmental defects
- Infections
- Inherited metabolic disorders
Investigations
No specific test can always confirm or exclude a diagnosis of HIE, since a diagnosis of HIE is made base on the history and physical and neurological examinations. Many of the tests are performed to assess the severity of brain injury and to monitor the functional status of systemic organs. As always, the results of the tests should be interpreted in conjunction with the clinical history and the findings from physical examination
- Serum electrolytes: In severe HIE cases, daily assessment of serum electrolytes are of value until the infant’s status improves. Markedly low serum sodium, potassium, and chloride in the presence of reduced urine flow and excessive weight gain may indicate acute tubular damage or Syndrome of Inappropriate Antidiuretic Hormone (SIADH), particularly during the initial 2-3 days of life.
- Renal function studies: Serum creatinine, creatinine clearance, and BUN. Creatinine increases 2-4 days after insult.
- Cardiac and liver enzymes values are an adjunct to assess the degree of hypoxic-ischemic injury to these other organs. Increased AST, ALT, PT, PTT, Albumin, Bilirubin and ammonia
- FBC and coagulation studies.
- Imaging Studies: cranial uss, CT scan, MRI.
- EEG to evaluate seizure activity
Treatment and Management of Birth asphyxia
Birth asphyxia is a perinatal emergency that requires quick clinical evaluation and prompt treatment
- Maintain body temperature by wiping baby dry and wrap up with warm towe or use of overhead radiant warmer
- Clear airway by gentle oropharyngeal and naso-pharygneal suctioning
- Use of Bag and face mask ventilation with weak respiratory activity or poor skin color
- Supplement face mask ventilation with oxygen therapy
- Endotracheal intubation when there is weak respiratory activity or ineffective bag and mask ventilation
- Cardiac resuscitation should be carried out with persistent heart rate below 80 beats per minute
- Drugs
a) Adrenaline 0.1-0.3 mg/kg of 1:10,000 solution by intravenous route
b) Naloxone Hydrochloride (maternal narcotic within 4hrs of delivery) by 0.1mg/kg Intravenous or Subcutaneous or intramuscular routes
c) Dextrose after prolonged resuscitation especially in: Asphyxia, Preterm infants or Infants of Diabetic Mothers (IDM). Dextrose is given by 1-2 ml/kg of 10% Dextrose/Water and 60-80ml/Kg/24hrs maintenance Intravenous fluid
d) Sodium hydrogen carbonate (NaHCO3) can be used for correction of acidosis. This is used only after respiration is established because CO2 can further depress the respiration.
e) 10% Calcium gluconate using 0.5-1ml/Kg diluted and given by Intravenous route slowly
f) Phenobarbitone (in HIE) using 20mg/Kg loading dose stat and then 8mg/Kg/day for 48-72 hrs
Further Medical care
Treatment of seizures is an essential component of management. Seizures should be treated with Phenobarbital or Lorazepam; Phenytoin may be added if either of these medications fails to control the seizures.
General Medical care for Birth asphyxia
No specific therapy for HIE exist. After seizure control, supportive care remains the cornerstone of management.
Supportive treatment of birth asphyxia
The elements of supportive care are as follows:
- Maintain adequate ventilation, perfusion, and metabolic status; most HIE infants need ventilator support during the first week.
- Prevent hypoxia, hypercapnia and hypocapnia; the latter is due to inadvertent hyperventilation, which may lead to severe hypotension of the brain.
- Maintain the blood gases and acid-base status in the physiological ranges including partial pressure of arterial oxygen (PaO2), 80-100 mmHg; partial pressure of arterial carbon dioxide (PaCo2), 35-40 mmHg and PH, 7.35 7.45
- Maintain the mean Blood pressure above 35mmHg (for term infants). Dopamine or doputamine can be used to maintain adequate cardiac output.
- Fluid, electrolyte and nutritional status should be monitored and corrected and adequate calories and proteins provided.
- Avoid hypoglycemia or hyperglycemia, as both are known to cause brain injury.
- In the first 2 days of life, restrict intravenous fluid to two thirds of the daily requirement for gestational age and nursing environment in light of the high frequency of acute tubular necrosis and IADH
- Individualize fluid and electrolyte therapy on the basis of clinical course, changes in weight, urine output, and results of serum electrolyte and renal function studies.
- When infants begin to improve, urinary output increases, and fluid administration must be adjusted. Similarly, in high-output renal tubular failure, the fluid volume and electrolyte composition need to be adjusted. For infants of high frequency ventilators, the administered fluid volume must be increased, since in those infants, venous return may be impaired, affecting cardiac preload.
Surgical care
In cases of posterior cranial fossa hematoma, surgical drainage may be lifesaving, if no additional pathologies exist.
CONSULTATIONS
A pediatric neurologist should help assist in the management of seizures, interpretation of EEG and overall care of the infant with HIE. The neurologist should also work with the PCP to address log-term disabilities. A developmental specialist also can help plan for long term assessments and care
DIET
In most cases (particularly in moderately severe and severe HIE), the infant is allowed nil per Os (NPO) during the first 3 days of life or until the general level of alertness and consciousness improves. Begin trophic feeding with dilute formula or expressed breast milk, about 5 ml every 3-4 hours.
Monitor abdominal girth and the composition of stools and signs of gastric retention; any of these may be an early indicator of necrotizing enterocolitis, for which infants with perinatal asphyxia are at high risk. Individualize increments in feeding volume and composition.
MEDICAL/LEGAL PITFALL
Avoid inappropriate designation of the diagnosis as asphyxia and ascribing asphyxia as a cause of any neurological symptom. The medical records should contain objective information on maternal and neonatal history and on clinical findings on the infant.
The results of any brain imaging procedures that have been carried out must be included in the total assessment of the infants clinical status. The findings of neuroimaging tests and EEG (if performed) must be documented. No diagnostic tests conclusively prove that a given magnitude of asphyxia has led to a specific neurological injury. Acute perinatal and intrapartum events have been found in only about 20% of children diagnosed as having cerebral palsy.
Parents must be given realistic explanations about their infants clinical status and prognosis. It should be emphasized that, except under controlled experimental conditions, cause-and-effect is nearly impossible to establish. Good medical records are always better than poor medical records: all details about the infants status and parental counseling must be documented carefully.
Predictors of Poor Neurodevelopmental outcome in Birth asphyxia
- Failure to establish respiration by 5 minutes
- Apgar 3 or less in 5 mts
- Onset of seizure in 12 hrs
- Refractory convulsion
- Stage III HIE
- Inability to establish oral feed by 1 weekk
- Abnormal EEG & failure to normalize by 7 days of life
- Abnormal CT. MRI, MR spectroscopy in neonatal period
Prevention of Birth asphyxia
- Good Antenatal care (ANC)
- Inform the neonatologist of a high risk delivery; A neonatologist experienced in neonatal resuscitation should be
- Immediate and adequate correction of fluid and electrolyte imbalances
- Counseling of Parents
- Follow up
- Rehabilitation of affected infants
Complications and long term effects of birth asphyxia:
- Hearing and speech deficit
- Seizure disorders
- Cerebral palsy
- Mental retardation
- Learning difficulties
- Attention deficit disorders
Detection of infants at risk of perinatal asphyxia:
- Fetal movement counting
- Non-stress testing
- Fetal biophysical profile
- Abnormal fetal heart rate (FHR) recording
- Fetal scalp pH
- Reduction of liquor volume
- Meconium staining of the liquor
Prognosis of birth asphyxia
Accurate prediction of the severity of long-term complications is difficult, although the following pointers may be used:
- Lack of spontaneous respiratory effort within 20-30 minutes of birth is associated with almost uniform mortality.
- The presence of seizures is an ominous sign. The risk of poor neurological outcome is distinctly greater in such infants, particularly if seizures occur frequently and are difficult to control.
- Abnormal clinical neurological findings persisting beyond the first 7-10 days of life usually indicate poor prognosis. Among these, abnormalities of muscle tone and posture (hypotonia, rigidity, weakness) should be carefully noted.
- An EEG done at about 7 days that has normal background activity is a good prognostic sign.
- Persistent feeding difficulties, which generally are due to abnormal tone of the muscles of sucking and swallowing, also suggest significant CNS damage.
- Head growth during the postnatal period and the first year of life is a sensitive finding predicting higher frequency of neurologic deficits.
- Counseling the parents with realistic explanations about their infant’s clinical status and prognosis is always recommended.
Perinatal/Birth asphyxia may result in fetal demise, neonatal death, or a period of recovery during which there is organ dysfunction with possible long-term effects, particularly in neurological function such as HIE.