Table of Contents
- Placental Abruption (Abruptio Placentae Definition)
- What is Placental abruption?
- Classification of Placental Abruption (Abruptio Placentae Types)
- Grading of Abruptio Placentae
- What Causes Placental Abruption (Risk factors of Placental Abruption)
- Placental Abruption Symptoms
- Signs of Placental Abruption
- Laboratory Investigations for diagnosis and Management of Placenta abruption
- Placental Abruption Treatment
- Differential diagnosis of Abruptio Placentae
- Maternal Complications of Placental Abruption
- Fetal Complications of Placental Abruption
Placental Abruption (Abruptio Placentae Definition)
Placental Abruption (also known as Accidental hemorrhage or Abruptio Placentae) is defined as bleeding from the placental bed of a normally sited placenta after 28 weeks of pregnancy.
What is Placental abruption?
Placental abruption is also known as Abruptio Placentae is one of the causes of Antepartum Hemorrhage and it refers to the premature separation of placenta after the age of viability (age of viability is 28 weeks of gestation or more). Placental separation may be complete or partial and when this occurs, it causes uterine bleeding.
Classification of Placental Abruption (Abruptio Placentae Types)
- Revealed Abruptio Placentae
- Concealed Abruptio Placentae
- Mixed Abruptio Placentae
Revealed Abruptio Placentae
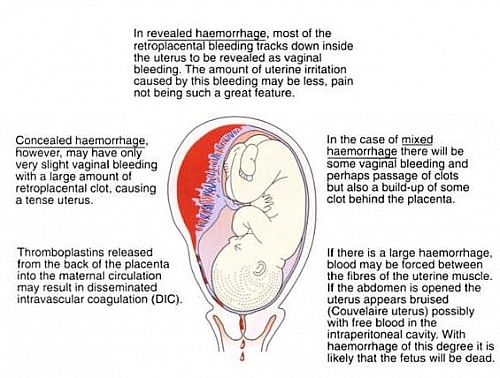
This is the commonest type of Abruptio Placentae whereby blood escapes through the potential space between the chorion and the decidua until it reaches the cervix.
Concealed Abruptio Placentae
This type of Abruptio Placentae shows no visible blood because blood is retained behind the decidua basalis and serosa. In this type, abdominal examination will give rise to a hard and tender uterus. At surgery the uterus shows a bluish discoloration (this is referred to as a Courvelaire Uterus); because the bleeding is concealed, this type of Abruptio Placentae usually presents with shock.
Mixed Abruptio Placentae
This is a combination of the revealed and concealed Abruptio Placentae. There will be some vaginal bleeding and perhaps passage of clots but also a build-up of some clot behind the placenta
Grading of Abruptio Placentae
- Grade 1 Abruptio Placentae: this grade is asymptomatic or retroplacental clot seen after birth under running water or on ultrasound scan.
- Grade 2 Abruptio Placentae: this is symptomatic; Foetus is alive and mother is hemodynamically stable.
- Grade 3 Abruptio Placentae: symptomatic; foetus is dead and mother is hemodynamically unstable. Grade 3A (there is no coagulability) and Grade 3B (there is coagulability)
What Causes Placental Abruption (Risk factors of Placental Abruption)
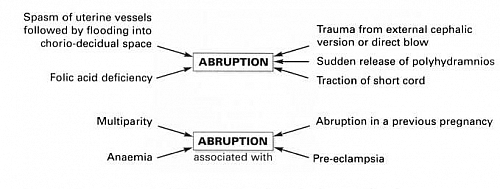
- Hypertension (including non proteinuric Pregnancy-induced hypertension and preexisting hypertension) about 30% due to spasm and degenerative changes in the decidual arterioles.
- Severe Preeclampsia and Eclampsia
- Direct trauma to the abdomen
- Multiparity (giving birth several times)
- Uterine over-distension which may be caused by Polyhydramnios or Multiple pregnancy (twins, triplets etc)
- Uterine fibroids
- Torsion of the uterus
- Folate deficiency and may be vitamin C,K, or E deficiency
- Short umbilical cord
- Sudden drop of intrauterine pressure such as in rupture of membranes in polyhydramnios
- The use of cocaine. Especially among pregnant women in most developed countries
- Chorioamnionitis
- Smoking
- Bleeding disorders
- External cephalic version
Placental Abruption Symptoms
- Vaginal bleeding that is dark red and clotted
- Severe abdominal pain
- Backache
- Sweating and dizziness (symptoms of shock especially from the concealed type).
Signs of Placental Abruption
- Cold clammy extremities (Hands and feet become cold)
- Rapid and thread pulse
- Pallor (patient becomes pale)
- Low blood pressure
- Tender woody and hard uterus on abdominal examination (in the concealed type of Abruptio Placentae)
- There may be increasing fundal height due to retained clots
Placental Abruption Ultrasound Findings
Placenta abruption ultrasound diagnosis depends on the formation of retroplacental clot or hematoma. If the hematoma is fresh, it will show acoustic characteristics very similar to those of the placenta itself. In less severe cases in which the pregnancy continues, the clot becomes increasingly echo-free with time and therefore more diagnostic. The ultrasound scan also helps to locate the placenta, exclude placenta previa and confirm fetal wellbeing.
Laboratory Investigations for diagnosis and Management of Placenta abruption
- Packed cell volume (PCV) to know the level of bleeding
- Confirmation of placental separation may be obtained by a positive Kleihauer test, indicating feto-maternal bleeding
- Group and cross match blood for transfusion
- Do Electrolyte, Urea and Creatinine levels (E,U,Cr) to rule out Acute Kidney Injury (AKI)
- Do Urinalysis for Protein in order to rule out Pregnancy Induced Hypertension (PIH)
- Do coagulation profile to rule out Disseminated intravascular coagulopathy (DIC)
- Do an obstetric ultrasound which will show retroplacental clot
Placental Abruption Treatment
Major placental abruption can be life-threatening for both the mother and the baby. Treatment approach depends on whether the baby is alive or death.
Management of Abruptio Placentae with a Live Fetus
- Insert two large-bore I.V cannulas and infusion of normal saline/colloid
- Send 20ml blood for cross-match of 4 units, haemoglobin and coagulation studies
- Perform an immediate Caesarean section if necessary to save the babys life (high risk of post-partum haemorrhage)
- Ensure adequate fluid replacement following the Caesarean section
- Leave an indwelling urinary catheter in to monitor urinary output
- Consider insertion of a central line to monitor maternal intravascular volume more closely
Management of Abruptio Placentae with a dead Fetus
When the fetus is dead, the woman should be allowed to deliver via vaginal delivery. Vaginal delivery usually happens rapidly (within 46 hours) as the placental abruption stimulates labour. If the woman does not go into labour then the membranes should be ruptured as this leads to a swift delivery.
Epidural analgesia is contraindicated because of the risk of Coagulopathy. If a coagulopathy develops (prolonged APTT, PTT, increased fibrin degradation products, low platelets) or the woman starts to bleed, she should be managed by giving 4 units of fresh frozen plasma with about 6 units of platelets ready. The consumptive coagulopathy begins to improve immediately after the uterus has been evacuated of its contents while marked abnormalities of the coagulation tests usually resolve within 46 hours following the delivery of the placenta.
There may be poor retraction of the uterus following the delivery of the placenta in abruptio placentae due to high levels of circulating fibrin degradation products, and thus an atonic postpartum haemorrhage may add to the dangers the mother already faces. Intravenous Oxytocics such as ergometrine is the drug of choice because of its tonic action on the uterus.
Differential diagnosis of Abruptio Placentae
- Placenta Previa
- Ruptured uterus because it also presents with abdominal pain
- Red degeneration of Uterine fibroid
- Peritonitis from perforated peptic ulcer disease (PUD) or appendicitis
- Acute Polyhydramnios
Maternal Complications of Placental Abruption
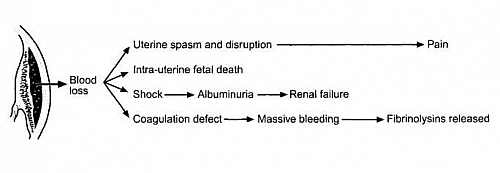
- Postpartum hemorrhage (PPH)
- Hypovolemic shock
- Disseminated intravascular coagulopathy (DIC)
- Acute Kidney Injury (AKI)
- Acute Cor pulmonale
- Sheehans syndrome
- Death
Fetal Complications of Placental Abruption
- Intrauterine Growth Restriction (lUGR)
- Perinatal Mortality