Table of Contents
- What is Pulmonary Tuberculosis (PTB)?
- Pulmonary Tuberculosis Epidemiology
- Pulmonary Tuberculosis Pathophysiology
- Pulmonary Tuberculosis Causes (Etiology)
- Pulmonary Tuberculosis Risk factors
- Pulmonary Tuberculosis Transmission
- Pulmonary Tuberculosis Symptoms
- Pulmonary Tuberculosis Signs
- Pulmonary Tuberculosis Test and Diagnosis
- Pulmonary Tuberculosis Radiology: Chest X ray findings in TB
- Pulmonary Tuberculosis Differential Diagnosis
- Pulmonary Tuberculosis Classification
- Pulmonary Tuberculosis Treatment Guidelines
- Pulmonary Tuberculosis Follow up
- Pulmonary Tuberculosis Complications
- Prevention of Pulmonary Tuberculosis
What is Pulmonary Tuberculosis (PTB)?
Pulmonary Tuberculosis is an infectious disease that affects the lungs. Pulmonary Tuberculosis is caused by a microorganism known as Mycobacterium tuberculosis which is an acid fast bacterium. Any form of Tuberculosis occurring outside the lungs is called Extrapulmonary Tuberculosis and there are various forms. Pulmonary tuberculosis is the most common form of tuberculosis: others include Tb Spine (Potts Disease), Miliary TB, Renal TB etc.
Pulmonary Tuberculosis Epidemiology
Tuberculosis is second leading cause of death caused by a single infectious disease, with 1.7 million deaths (without HIV infection) in 2004. It affects one third of the worlds population and 95% of TB causes are in the developing countries. Most cases of Tuberculosis in developed countries affect the elderly while in developing countries affect people within the ages of 15 to 50 years. Tuberculosis is an important cause of morbidity and mortality.
Pulmonary Tuberculosis Pathophysiology
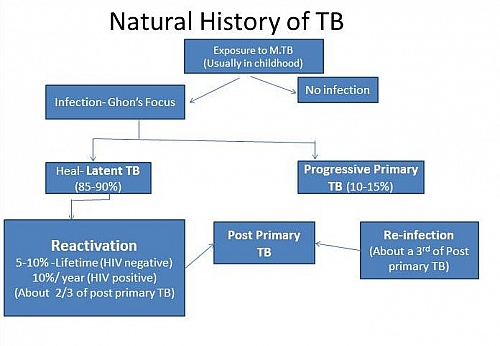
When a person gets exposed to the tubercle bacilli for the first time, a Primary Tuberculosis infection results and this usually occurs in children and it is made up of parenchymal lesion and hilar lymph node enlargement. Following inhalation of the infective droplets of the tubercle bacilli, most are deposited in the upper airway and are cleared by the ciliated mucosal cells with only a fraction getting to the alveoli. The bacilli are usually deposited in the sub-pleural part of the lungs.
In the alveoli of the lungs, the tubercle bacilli are ingested by non-specifically activated alveolar macrophages and phagocytosis of the bacilli sets up an inflammatory response involving monocytes, CD4+ T lymphocytes and subsequently, activated macrophages with specific activity against Mycobacterium tuberculosis.With the development of specific immunity and accumulation of a large number of activated macrophages at the site of the primary lesion, granulomatous lesions are formed called the Ghons focus. Infected macrophages could carry this infection to the draining lymph nodes forming the primary complex.
This primary infection goes undetected because of the bodys immunity (in a person with normal immunity); it is usually self-limiting and heals with calcification. However when there is low immunity primary infection progresses to clinical disease (progressive primary tuberculosis).Pulmonary Tuberculosis disease in adults is usually due to re-activation of a primary infection and usually symptomatic. This is called post primary tuberculosis.
Pulmonary Tuberculosis Causes (Etiology)
- Mycobacterium tuberculosis
- Mycobacterium bovis
- Mycobacterium africanus
- Mycobacterium avium
Mycobacteria comprise of a large group of acid fast, alcohol fast, aerobic or microaerophilic, non-spore-forming and non-motile bacilli. Tubercle bacilli are difficult to stain but once stained strongly retain the dye, which is not removed by acid alcohol solution.
Pulmonary Tuberculosis Risk factors
- HIV/Aids infection is currently the most important risk factor for developing tuberculosis with about 30% of TB patients having HIV co-infection. This is why HIV test is required in patients having tuberculosis.
- Overcrowding such as in refugees and prisoners
- Malnutrition such as in Kwashiorkor and Marasmus
- Alcohol abuse
- Chronic renal failure
- Organ transplant
- Immunosuppression states such as in Diabetes Mellitus, Malignancies, pregnancy, and long term use of steroids
- Exposure to biomass fuel
Pulmonary Tuberculosis Transmission
Mode of Transmission of Pulmonary Tuberculosis occurs through inhalation of air droplets containing the tubercle bacilli. TB transmission occurs when an individual with active pulmonary Tuberculosis coughs, laughs, sings, speaks or sneezes and another person inhales the droplets. Pulmonary TB is therefore an airborne disease and is communicable. Tiny infectious droplets once produced are distributed in the air and can survive for long periods in a dark poorly ventilated room; the tubercle bacilli are easily destroyed by sunlight (ultraviolet rays).
Another mode of transmission of Pulmonary Tuberculosis occurs by consumption of unpasteurized milk (cows milk) from a cow infected with mycobacterium bovi.
Pulmonary Tuberculosis Symptoms
- Chronic cough of more than 3 weeks that is productive of mucoid sputum which may be blood stained
- Weight loss
- Fever- usually low grade with evening chills
- Drenching night sweat
- There may be chest and dyspnea
Pulmonary Tuberculosis Signs
- Low grade fever
- Anemia
- Varying degrees of dyspnea (difficulty in breathing)
Pulmonary Tuberculosis Test and Diagnosis
- Sputum microscopy: for Acid fast bacilli (AFB) this is the most important pulmonary tuberculosis test when PTB is suspected. In areas of high TB endemicity, a positive AFB smear is highly suggestive of Pulmonary Tuberculosis. 3 samples are usually collected over two days such as one sample at the spot, then in the morning of the next day and then a third sample when the patient sees the doctor during the day (spot-morning-spot samples)
- Chest X-ray: chest radiology in pulmonary tuberculosis typically shows apical fibrosis; there may be cavitations, fibrosis, pleural effusion etc.
- Full Blood Count (FBC): there may be Lymphocytosis and anemia
- Erythrocyte Sedimentation Rate (ESR): this will be elevated. Normal ESR in males is calculated by dividing the age of the patient by 2 (that is ESR= age/2); Normal ESR in females is calculated by adding 10 to the age and then dividing the sum by 2 (that is, [age+10]/2)
- Tuberculin skin test: this must be interpreted with caution putting into consideration the associated morbidities and health status of the patient. This has been extensively explained in this article about Tuberculin skin test. It is based on a delayed hypersensitivity reaction following previous exposure to the tubercle bacilli. The tuberculin skin test could be Mantoux test (which is still in use), Heaf test no longer in use or Tine test no longer in use too.
- Culture: using solid media such as Lowenstein Jensen media or liquid media such as BACTEC
- Polymerase Chain Reaction (PCR) based tests for Pulmonary tuberculosis using GeneXpert MTB/RIF. This can also be used to test for Rifampicin resistance.
- Biopsy of various organs such as lymph node
- Liver function tests to check for AST, ALT, and Bilirubin levels
Pulmonary Tuberculosis Radiology: Chest X ray findings in TB
- Commonly affects apical or posterior segment of right upper lobe, superior segment of either lobe or apico-posterior segment of left upper lobe. In cases of reactivation pulmonary TB, cavitary upper lobe disease is common.
- Presence of fibronodular shadows and cavitations
- Presence of Hilar adenopathy common in HIV infected persons and young children.
- Pulmonary TB may exist but chest X-ray finding may be normal or only mildly abnormal especially in HIV patients.
Pulmonary Tuberculosis Differential Diagnosis
- Pneumonia
- Chronic Obstructive Pulmonary Disease (COPD)
- Asthma
- Heart failure
- Bronchiectasis
Pulmonary Tuberculosis Classification
World health organization (WHO) classified TB patients to help in their treatment.
WHO Category of Tuberculosis disease
- Category 1: a new TB case
- Category 2: Re-treatment case
- Category 3: sputum smear negative; not seriously ill but with Extrapulmonary Tuberculosis
- Category 4: a multidrug resistance TB (MDR TB)
Pulmonary Tuberculosis Treatment Guidelines
The treatment for pulmonary tuberculosis is based on the standard TB treatment and it is done using the world health organization (WHO) classification of TB patients to different categories.
The DOTS – Directly Observed Therapy Short course is used and it has 2 Phases of treatment: the Intensive phase and Continuation phase.
Pulmonary Tuberculosis Treatment Guideline for Category 1 Patients
- Intensive Phase: this lasts for 2 months (8 weeks) and the drugs used include Rifampicin, Isoniazid, Ethambutol and Pyrazinamide.
- Continuation Phase: this lasts for 4 months (16 weeks) and drugs used include Rifampicin and Isoniazid
Pulmonary Tuberculosis Treatment Guideline for Category 2 patients
- Intensive Phase: this phase for category 2 patients lasts for 3 months Streptomycin is used for the first 2 months and Rifampicin, Isoniazid, Ethambutol and Pyrazinamide in the 3rd month.
- Continuation Phase: this lasts for 5 months (20 weeks) and drugs used include Rifampicin, Isoniazid and Ethambutol
Pulmonary Tuberculosis Treatment Guideline for Multi drug resistant tuberculosis (MDR TB)
Multi drug resistant Tuberculosis (MDR TB) is the resistance to at least Rifampicin and Isoniazid. Treatment of this type of TB requires the use of second-line TB drugs and should be supervised by a specialist. The Treatment duration for MDR TB is between 18 and 24 months.
List and names of Second line Tuberculosis Drugs for MDR TB
- Rifabutin
- Azithromycin
- Capreomycin
- Clarithromycin
- Ofloxacin
- Ciprofloxacin
- Amikacin
- Kanamycin
- Cycloserine
Names and List of Drugs for Standard Treatment of Pulmonary Tuberculosis
- Rifampicin
- Isoniazid
- Pyrazinamide
- Ethambutol
- Streptomycin
- Para Amino Salicylic Acid (PAS)
Pulmonary Tuberculosis Follow up
Follow up of Pulmonary Tuberculosis involves reviewing the symptoms and signs of Pulmonary Tuberculosis and carrying out physical examination and tests to monitor the respond to treatment or progress of the disease.
Parameters to check on Pulmonary Tuberculosis Follow up
- Regular weighing of the patient
- Serial sputum AFB staining
- Serial ESR estimation
- Full blood count (FBC)
- Chest X ray
Pulmonary Tuberculosis Complications
- Aspergilloma
- Bronchiectasis
- Broncholithiasis
- Fibrothorax
- Massive hemoptysis (coughing of blood)
- Pneumothorax
- Cor-Pulmonale (Right heart failure)
- Respiratory Failure
Prevention of Pulmonary Tuberculosis
- Good nutrition
- Good ventilation
- Avoid overcrowding
- Avoid contact with chronically coughing individuals
- Good social conditions
- Vaccination in Children