Table of Contents
- What is Drug Resistant Tuberculosis?
- What causes Drug Resistant Tuberculosis?
- Types of Drug Resistant Tuberculosis (Classification of drug resistance in TB)
- Difference between simple drug resistance TB and Multidrug resistant TB
- Drug Resistant Tuberculosis Treatment Guidelines
- Tuberculosis Treatment regimen where Multidrug Resistant Tuberculosis (MDR TB) is known from culture result
- Tuberculosis Treatment regimen when no culture results are available
- Tuberculosis Treatment Failure
- Tuberculosis Treatment Relapse
- New Case of Tuberculosis
- Return after interruption of treatment (Default)
- Is it possible to cure MDR TB?
What is Drug Resistant Tuberculosis?
Drug resistant Tuberculosis refers to a case of TB (which is mostly pulmonary Tuberculosis) in which the patient is excreting bacilli resistant to one or more anti tuberculosis drugs; All TB patients have some naturally resistant strains of TB bacilli. Resistance to Isoniazid is about 1 in 106 cases of TB while resistance to Rifampicin is about 1 in 108 cases of TB. Developing resistance to both Rifampicin and Isoniazid is about 1 in 1014 cases of Tuberculosis.
What causes Drug Resistant Tuberculosis?
Drug ResistantTuberculosis is caused by chromosomal mutation of the bacilli. Clinical drug resistance is caused by human creation as a result of poor treatment or irregular treatment; by doing this, naturally resistant bacilli are therefore selected out and amplified until they are dominant population amongst the TB bacilli.
Types of Drug Resistant Tuberculosis (Classification of drug resistance in TB)
- Primary Drug Resistance this type of resistant tuberculosis is produced by being infected with a drug resistant tuberculosis strain. When you get infected with TB from someone who has a resistant type of TB (either because the person did not take his or her drugs well or because he or she was also infected with a resistant type of TB from someone else), then you also will have drug resistant TB too. This form of resistance is found in a patient who has no history of prior anti TB drug treatment.
- Acquired Drug Resistance this is type of resistant tuberculosis is produced by ineffective Tuberculosis treatment. This type of resistance is found in a patient who has received at least 1 month of prior anti TB treatment.
- Simple drug resistance Tuberculosis (SDR TB) this refers to resistance to more than two first line drugs including isoniazid or rifampicin. When you are resistant to treatment to 3 or more of these antituberculosis drugs (Rifampicin, Isoniazid, Ethambtol, Pyrazinamide and Streptomycin), then you are said to have a simple drug resistant TB;
- Multidrug-resistance (MDR) this refers to resistance to more than two first line drugs including both isoniasid and rifampicin
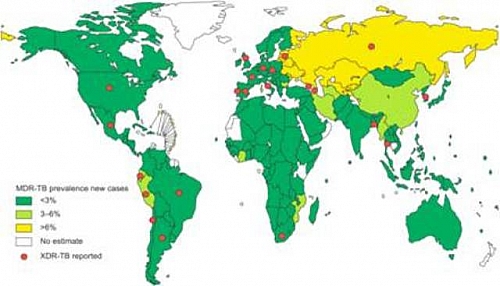
- Extensively Drug Resistance Tuberculosis (XDR TB) this is a resistance to Rifampicin and Isoniazid and also to at least some fluoroquinolones and one from 3 injectional antituberculosis drugs: cyclopentin, kanamycin, amikacin.
Difference between simple drug resistance TB and Multidrug resistant TB
- Multidrug resistant TB is includes developing resistance to both Rifampicin and Isoniazid (that is, resistance must be developed to all the two drugs: Rifampicin and Isoniazid at the same time) with or without other first line TB drugs
- Simple drug resistant TB involves developing resistance to either Rifampicin and two or more other first line TB drugs or developing resistance to Isoniazid and two or more other first line TB drugs
Drug Resistant Tuberculosis Treatment Guidelines
- In isolated Isoniazid resistance use Ethambutol, Rifampicin and Pyrazinamide for 6 months
- In Rifampicin resistance use Ethambtol and Isoniazid for 18 months
- In multidrug resistance use Streptomycin, Isoniazid and Pyrazinamide for 9 months
- In resistance to Isoniazid, Rifampicin and Streptomycin resistance use Pyrazinamide, Ethambutol with Ofloxacin or Ciprofloxacin and Amikacin for 18 to 24 months
- Isoniazid, Ethambutol, Rifampicin and Streptomycin resistance use Pyrazinamide with Ofloxacin or Ciprofloxacin, Amikacin and 2 other second line TB drugs for 24 months
- Isoniazid, Ethambutol , Pyrazinamide and Streptomycin resistance use Ethambutol with Ofloxacin or Ciprofloxacin, Amikacin and 2 other second line TB drugs for 24 months
- Isoniazid, Ethambutol, Pyrazinamide, Rifampicin and Streptomycin resistance use Ofloxacin or Ciprofloxacin, Amikacin and 2 other second line TB drugs for 24 months
These treatment guidelines are based on culture results and susceptibility tests.
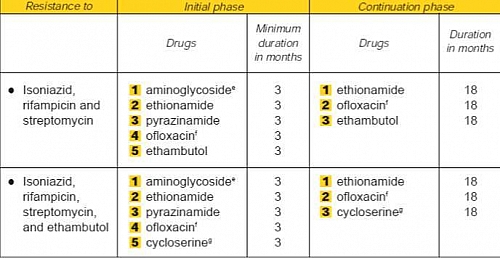
Tuberculosis Treatment regimen where Multidrug Resistant Tuberculosis (MDR TB) is known from culture result
- Intensive phase: this is done in 3 months using Aminoglycoside (Kanamcin,Amikacin or Capreomycin), Ethionamide, Pyrazinamide, Ofloxacin and Ethambutol
- Continuation phase for 18 months using Ethionamide, Ofloxacin and Ethambutol
If resistance to Ethambutol is present, use cycloserine or PAS if available
Tuberculosis Treatment regimen when no culture results are available
- Intensive phase treatment for 3 months using Aminoglycoside (kanamycin, amikacin or capreomycin), Ethionamide, Pyrazinamide and Ofloxacin
- Continuation phase treatment for 18 months using Ethionamide and Ofloxacin
Tuberculosis Treatment Failure
Treatment failure in TB refers to a patient who is still excreting bacilli either after 5 months of chemotherapy given under direct observation by a health worker or after completion of the fully supervised 8 month retreatment regimen (with 2 months treatment with Streptomycin, Rifampicin, Isoniazid, Ethambutol and Pyrazinamide; 1 month with Rifampicin, Isoniazid, Ethambutol and Pyrazinamide and then 5 months with Rifampicin, Isoniazid and Ethambutol.
Tuberculosis Treatment Relapse
Treatment relapse TB occurs in a patient who previously received treatment and was declared cured and has once again developed sputum smear positive TB within 1 year.
New Case of Tuberculosis
A new case of TB refers to patient who has never had treatment for TB or who has taken anti TB drugs for less than 4 weeks
Return after interruption of treatment (Default)
This refers to a new TB patient who completed at least 1 month of treatment and returned smear positive after at least 2 months interruption of treatment.
Is it possible to cure MDR TB?
Multidrug Resistant Tuberculosis (MDR TB) can be cured when there is compliance but can also be fatal especially when the patient fails to comply with the drugs again. It must be made clear to the patient and staff that meticulously taking the prescribed reserve regimen is all that stands between the patient and death.