Gastrointestinal (GI) bleeding refers to loss of blood from the gastrointestinal tract. It is also known as GastroIntestinal hemorrhage. Bleeding from the GI tract can be in the form of throwing up blood (Vomiting blood), passing melena stool (dark tarry stool) or even passing of fresh bright red blood in stool. GI bleeding is not a medical condition but a symptom caused by certain diseases. This article will talk about these diseases that cause GI bleeding. Their symptoms can be used to know the nature of the bleeding, the cause of the bleeding and the necessary treatment needed to save the life of the affected person.
Before you understand GI bleeding, you need to know the structure of the gastrointestinal tract. The picture of the GI tract can be seen below. The GI tract consists of the mouth, the esophagus, the stomach, the duodenum, the jejenum, ileum, colon, cecum, rectum and anus. The duodenum, jejenum and ileum are together referred to as the small intestines; the colon, cecum and rectum are the large intestines.GI bleeding can occur in any of the above listed parts of the GI tract; hence, you could have stomach bleeding, mouth bleeding, duodenal bleeding, jejunal bleeding, rectal bleeding or bleeding from colon.
Table of Contents
- Upper and Lower GI bleeding
- Epidemiology and Statistics of GI Bleeding
- GI Bleeding Risk factors
- GI Bleeding Causes
- Pathophysiology of specific causes of GI Bleeding
- GI Bleeding Symptoms and Signs
- Laboratory tests (investigations) to know the cause of GI bleeding and help in management
- Management and treatment of GI Bleeding
- GI Bleeding Complications
- Outcome of GI bleeding (Prognosis)
Upper and Lower GI bleeding
There may be upper GI bleeding and lower GI bleeding and one could know if the cause of the bleeding is from the upper parts of the intestine or lower parts of the intestinal tract. The junction between the duodenum and the Jejunum is known as the duodeno-jejunal junction and has a ligament known as the ligament of Treitz. This junction forms the demarcation or separation between the upper and lower Gastrointestinal tract. Any GI bleeding above the ligament of treitz is called Upper GI bleeding and when the bleeding is below the ligament, it is called Lower GI bleeding. The causes of Upper GI bleeding are different from that of the Lower GI bleeding and their management and symptoms are also different.
Epidemiology and Statistics of GI Bleeding
Depending on the country, the cause of bleeding from the gastrointestinal tract can be as a result of various factors. In most parts of Africa, peptic ulcer is the commonest cause; in some African countries like Tanzania and Zimbabwe, esophageal varices are the commonest cause than peptic ulcer. In the Unites States of America and United Kingdom, the common causes of GI Bleeding are as a result of Chronic Peptic Ulcer disease (in 50% of cases), Mallory Weiss tears in 13% of cases, stress ulcers accounts for 10% and esophageal varices for 2%.
GI Bleeding Risk factors
- Alcoholism: taking of much alcohol places you at risk of liver cirrhosis and Mallory Weiss syndrome. This is common in alcoholics.
- Use of Aspirin, Warfarin (Coumadin), Rivaroxaban (Xarelto) or Clopidogrel (Plavxi)
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) such as Ibuprofen and Feldene,
GI Bleeding Causes
Upper GI Bleeding Causes (Etiology)
- Duodenal ulcer
- Gastric ulcer
- Stress ulcer (due to gastric erosions or gastritis)
- Esophageal varices
- Esophagitis
- Mallory Weiss Syndrome
- Stomach Tumors (Malignant or Benign)
- Esophageal ulcer
- Esophageal cancer
- Hiatal hernia
- Duodenal tumors
- Pancreatic tumors
- Aneurysm of the abdominal aorta
- Blood dyscrasia
- Hereditary telangiectasia
- Angiodysplasia
- Dieulafoys lesions
Lower GI Bleeding Causes
- Diverticulosis
- Rectal varices
- Anal varices
- Inflammatory bowel disease
- Rectal tumors
- Colonic tumors
- Polyps
Pathophysiology of specific causes of GI Bleeding
Mallory-Weiss Syndrome: this occurs due to a tear of the part of the stomach and sometimes part of the esophagus leading to bleeding and vomiting of blood. It is usually caused by prolonged vomiting or retching that usually occurs in alcoholics; after drinking too much alcohol, it triggers vomiting which becomes prolonged with retching and a tear may occur, giving rise to Hematemesis (throwing up blood).
Dieulafoys lesions: these are rare but might cause massive and recurrent GI Bleeding without any known reason. The patient may throw up blood and even when the inside of the stomach and duodenum is viewed using an instrument known as an endoscope, nothing will be seen and the source of the bleeding cannot be ascertained. This is because the sources of the bleeding are very small and are not readily seen.
Esophageal varices: it refers to the dilation (distension) of veins of the esophagus as a result of portal hypertension. Portal hypertension can be caused by liver cirrhosis which may be a complication of Hepatitis B or C. When these veins become enlarged, they can rupture and massive GI bleeding occurs with vomiting of blood. This is an emergency that if not treated in time, the person may die.
Chronic Peptic Ulcer: this is a long standing peptic ulcer. It could be duodenal peptic ulcer or gastric peptic ulcer (stomach ulcer). Bleeding duodenal ulcer is commoner than gastric ulcer. Chronic Peptic ulcer is a common complication of peptic ulcer in the United Kingdom and the United States of America.
Stress Ulcer: this type of ulcer may result from severe burns, sepsis or trauma.
GI Bleeding Symptoms and Signs
- Vomiting of blood that may be coffee ground in color
- Passage of black tarry stool (melena stool)
- Passing bloody stool or stool covered with blood (known medically as Hematochezia)
- The patient may be pale looking due to significant loss of blood
- There could be sweating and the hands and feet become cold as a result of shock (a severe loss of blood). This is not a condition that can be treated at home. If nothing is done, the patient may go into coma and death may occur.
Laboratory tests (investigations) to know the cause of GI bleeding and help in management
- Full blood count: small pale red cells seen (microcytic and hypochromic) shows the bleeding is chronic (long standing).
- Prothrombin time shows whether the GI bleeding is due to defects in coagulation factors
- Renal profile: kidney failure and electrolyte disturbance as a result of the GI bleeding and throwing up blood may occur. Blood Urea Nitrogen (BUN) greater than 100 may further caused poor platelets function and predispose to bleeding.
- Liver function tests: if the cause of the GI bleeding is due to liver disease, the serum albumin will be low.
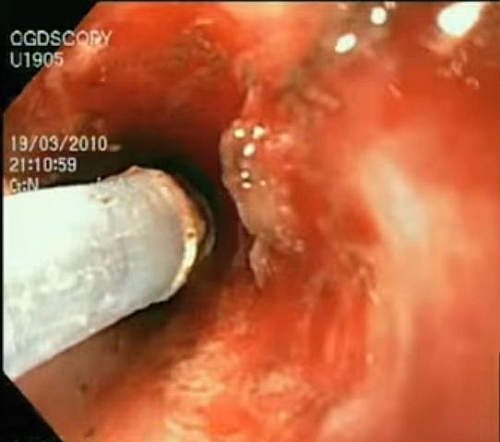
- Endoscopy (Esophago-gastro-duodenoscopy): this is a procedure where a small tube is inserted into the stomach and duodenum and it is used to view the intestinal tract up to the 2nd part of the duodenum. The inserted tube contains a camera that shows the inside of the gastrointestinal tract on a screen that looks like a TV. This procedure can be used for diagnosis of the source of the bleeding and can be used for taking biopsy samples for further investigations if malignancy (cancer of the stomach is suspected). It can also be used for stopping the bleeding by injecting adrenaline or a sclerosant. Endoscopy is done when the bleeding patient has been stabilized and gastric lavage has been thoroughly carried out to aid in visualization.
- Angiography can be used for therapeutic purpose for embolization (occluding the bleeding blood vessel.)
- Labeled red blood cell (RBC) scan can also be used; more sensitive than angiography and has less complications
- Barium meal helps to outline the GI tract and can show ulcers, tumors, and reflux esophagitis.
- Colonoscopy/Sigmoidoscopy help in visualization of the colon just like endoscopy
Management and treatment of GI Bleeding
In the management and treatment of gastrointestinal bleeding, the first thing will be to stabilize the patient. This is done in the hospital and never at home.
The patient is checked to see if he or she is breathing well. The airways are checked. If there is difficulty in breathing, oxygen is administered.
In order to replace the lost blood, two large bore canulae are set (size 14 or 16); blood is then taken for grouping and cross matching; crystalloids are given (fluids that are given to increase the blood volume before 6 units of blood are grouped and cross matched for blood transfusion). Urethral catheter is then place to monitor the amount of urine made by the patient. The vital signs such as Temperature, Respiration, blood pressure and Pulse rate are monitored.
A NasoGastric (NG) tube is then inserted into the stomach of the patient by passing it through the nose, esophagus and then the stomach. This NG tube helps to remove any blood in the stomach and prevents the patient from aspirating the vomited blood into the lungs. If bright red blood returns from the NG tube, it shows it is an ongoing GI bleeding. If the blood returned from NG tube is coffee ground, it shows that the patient has bled before coming and might have stopped.
Once the bleeding stops and the patient has been stabilized, then specific treatment is carried out depending on the cause of the GI bleeding.
Specific GI Bleeding Treatment
Peptic Ulcer Disease (PUD): Helicobacter Pylori (H. Pylori) is implicated in about 70% of cases of Peptic ulcer. The bacterium should be eradicated. Frequent milk feeds, antacids H2 Receptor antagonists such as ranitidine are given. Omeprazole is of more benefit than H2 Receptors blockers. Reducing the gastric acid helps promote ulcer healing. In massive bleeding, octreotide, a synthetic somatostatin analogue is given by infusion at a constant rate. Octreotide acts by inhibiting gastric acid secretion and enhances aggregation of platelets in order for clotting to occur in the bleeding vessel. Octreotide also reduces splanchnic blood flow by vasoconstriction and so is effective in stopping bleeding from esophageal varices too.
If there is significant loss of blood in which more than 5 units of blood are transfused within 24 hours, then surgery should be done. Endoscopic sclerotherapy or Electrocautery can be done especially in High risk patients. Elderly patients should have early surgical intervention. Vasopressin may be used to stop bleeding but should be avoided in patients with GI bleeding who also have Coronary Artery Disease (CAD) or recent Myocardial infarction (MI).
Stress Ulcers: treat underlying cause such as burns, sepsis or trauma. Gastric lavage, Antacids and H2 receptor antagonist (blockers) such as Ranitidine or Cimetidine may be given. If medical treatment fails, then surgery can be done such as Truncal vagotomy and Pyloroplasty or gastrectomy (partial or total)
Esophageal varices: administration of vasopressin (ADH) decreases the portal pressure but this should not be given to patients with CAD. Use of Sengstaken-Blakemore tube for 24 hours can also stop bleeding. Other treatment modalities are Endoscopic Sclerothreapy (or ligation with rubber band) or TransJugular Intrahepatic Portosystemic shunts.
Mallory Weiss Syndrome: majority of patients stop bleeding spontaneously, hence supportive treatment can be given. Endoscopy and Bipolar or Laser coagulation can be used if supportive treatment fails. Direct suturing can be done too.
GI Bleeding Complications
Complications could arise directly from the GI Bleeding such as Kidney failure, shock, coma or death; complications could arise from the surgical procedures while treating the patient; hence the need for proper stabilization of patient and adequate preparation before surgery.
Outcome of GI bleeding (Prognosis)
Generally, mortality of about 10 to 15% occurs in GI Bleeding but is increased to 33% in the elderly. Also, existing diseases (comorbidities) could increase the mortality rate.