Table of Contents
- Definition of Heart Failure
- What is Congestive Heart Failure
- Epidemiology of Heart failure
- Types of Heart Failure
- Causes/Etiology of Heart Failure
- Pathophysiology of Heart Failure
- Clinical features/Signs and Symptoms of Congestive Heart Failure
- Findings of Physical Examination in Heart Failure
- Framinghams criteria for diagnosis of Congestive Cardiac Failure
- Laboratory Investigations to confirm Heart Failure
- Differential diagnosis of Heart Failure
- Stages of Heart Failure
- Classification of Heart Failure
- Treatment of Heart Failure
- Complications of Congestive Heart Failure
- Prognosis of Heart Failure
Definition of Heart Failure
Heart failure (also known as Congestive Cardiac Failure, CCF or Congestive Heart Failure, CHF; they all mean the same) is a clinical syndrome characterized by inability of the heart to function as a pump to maintain the normal circulation of blood, or its ability to do so only in the presence of an elevated venous pressure.
What is Congestive Heart Failure
In Heart Failure, the heart cannot keep up its work load of pumping blood to the lungs and to the rest of the body. This occurs in patients who, because of an inherited or acquired abnormality of cardiac structure or function, develop a constellation of clinical symptoms (dyspnea and fatigue) and signs (edema and rales) that lead to frequent hospitalizations, a poor quality of life, and a shortened life expectancy.
When Heart failure occurs, the body tries to overcome it automatically but usually only worsens the condition. If the blood meant for less essential organs instead flows to the brain and other vital organs the heart has to work harder to get it to all parts of the body. When the activity of the heart is increased, a more forceful contraction causes an increased heart rate.
Epidemiology of Heart failure
Heart failure has a worldwide distribution, with more than 20 million people affected. Prevalence of 2% in developed regions, rising to 6 10% in populations of age more than 65yrs. It is estimated that as many as two million Americans suffer from congestive heart failure and that up to 29, 000 die annually from this chronic disorder. Prevalence is greater in males than in females for patients aged 40-75 years.
No sex predilection exists for patients older than 75 years. Prevalence of Congestive Heart Failure increases with increasing age and affects about 10% of the population older than 75 years.
The prevalence of heart failure is expected to rise in near future. It has a 50% mortality rate and accounts for 5% of all hospital admissions. Heart failure is the leading cause of hospitalization among those >65 and about 60% of those with heart failure are re-hospitalized within 6 months due to recurrent decompensation. The prevalence doubles each decade. The cost of Heart Failure roughly doubles that of any cancer diagnosis.
Types of Heart Failure
- Acute or chronic
- Left sided and/or right sided
- Diastolic and/or systolic
- High output or low output
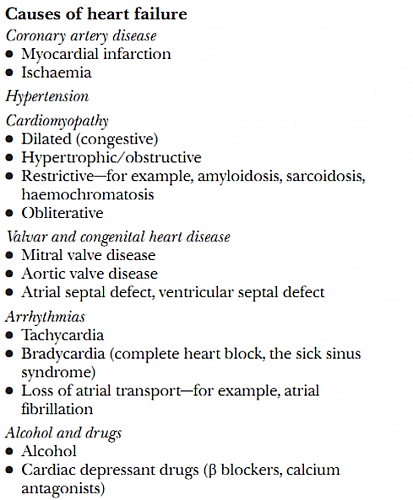
Causes/Etiology of Heart Failure
- Hypertension: often associated with left ventricular hypertrophy with preserved ejection fraction
- Cardiomyopathies such as:
– dilated(congestive) cardiomyopathies,
– obstructive (hypertrophic) cardiomyopathies,
– obliterative cardiomyopathies,
– restrictive cardiomyopathies (such as amyloidosis, sarcoidosis, and haemochromatosis) - Ischemic heart disease
- Myocardial infarction
- Valvular heart diseases
- Congenital heart diseases (CHD)
- Pericardial disease (Pericardial effusion, constrictive pericarditis)
- Anemia
- Thyroxicosis
- Hypothyroidism
- Phaeochromocytoma
- Pagets disease
- Cushings syndrome
- Alcoholic heart disease
- Toxic substances such as mercury, cobalt and arsenic poisoning
- Use of drugs such as beta blockers, cytotoxic drugs, cocaine and calcium antagonist
- Beri beri
- Previous heart attack
- Nutritional deficiencies such as thiamine (Vitamin B1) and selenium deficiencies
- Arrythmias: chronic rapid heartbeats ( such as Atrial Fibrillation)
- End stage renal failure
- Infections such as HIV/AIDS and Chagas disease
Congenital Heart Disease (CHD) as a cause of Heart Failure
CHD affects one out of every one thousand babies. In these babies the marvelously intricate combination of chambers, valves, and vessels making up the heart and circulatory systems fails to form properly before birth. Septal, atrial, and ventricular defects are the most common CHDs.
Rheumatic Fever
Sore throat from the streptococcal infection begins a disease process where the heart valves are damaged. This condition is called rheumatic fever and it affects the connective tissues of the body.
Cardiomyopathy causing Heart Failure
Cardiomyopathy is the stretching and enlarging of the heart cavity that occurs making the heart weak so it does not pump blood correctly leading to Congestive Heart Failure.
Ventricular Failure
Ventricular failure occurs when there are weak spots in the ventricular walls causing a bulge, or an aneurysm in the walls of the heart.
Atherosclerosis
Atherosclerosis is the gradual clogging of the arteries by fatty, fibrous deposits. A tiny lump of fibrous tissue grows as the artery tries to repair the damage. Cholesterol accumulates and more tissue builds up. The arteries are thickened and hardened making a loss of elasticity causing congestion.
Pathophysiology of Heart Failure
When myocardium fails, Cardiac Output drops, this leads to redistribution of blood, with peripheral vasoconstriction and renal hypoperfusion. This is sensed by the body as dehydration and Renin-Angiotensin-Aldosterone mechanism is stimulated to cause sodium and water retention and its sequelae. This worsens peripheral vasoconstriction, and increases preload on already failing heart and therefore worsens the work load of the heart because there will be congestion or pooling excess blood in the heart (hence it is often called Congestive heart failure instead of just heart failure).
Sympathetic overdrive, meant to increase cardiac output, leads to myocyte (heart muscles) apoptosis and Left Ventricular remodeling. The Failing heart releases natriuretic peptides to induce sodium loss and levels of this determine the prognosis of heart failure.
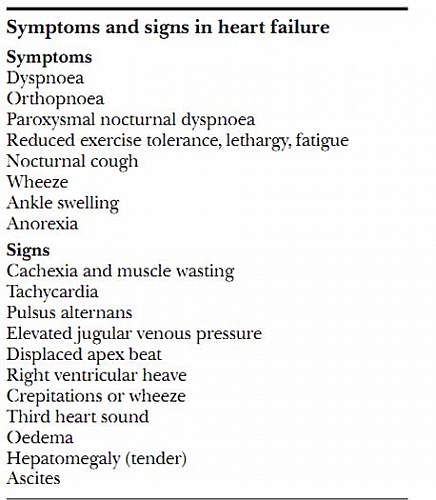
Clinical features/Signs and Symptoms of Congestive Heart Failure
- Dyspnea: difficulty in breathing; may start with exercise and later progresses to breathing problems even at rest.
- Fatigue: weakness of the body and feeling of tiredness
- Orthopnea: difficulty in breathing on lying down flat
- Paroxysmal Nocturnal Dyspnea (PND): difficulty in breathing especially at night while sleeping that makes you keep getting up from sleep because you feel as if you are breathless.
- Chronic Cough
- Leg, ankle and hand swelling
- Early satiety: feeling of fullness after eating little
- Right upper quadrant pain (abdominal pain)
- Abdominal distention (the abdomen swells as a result of fluids in a sac that lines the abdominal contents called the peritoneum
- Anorexia: loss of appetite
- Palpitations: feeling of your own heart beating fast; heart beat may be irregular.
- Chest pain
- Distension or engorgement of neck veins. The neck veins become prominent
- Cyanosis, or a bluish color that is seen in the lips and fingernails from a lack of oxygen
- Changes of behavior such as restlessness, confusion, and decreased attention span
Findings of Physical Examination in Heart Failure
- Cachexia
- Dyspnea
- Orthopnea
- Cyanosis
- Pedal and sacral edema
- Tachycardia
- Peripheral hypothermia
- Blood pressure reduces usually
- Jugular venous pulsation with elevated estimated JVP
- Displaced apex
- Added heart sounds, +/- murmurs
- Posterior basal crepitations, +/- pleural effusions
- Tender hepatomegaly
- Ascites
Framinghams criteria for diagnosis of Congestive Cardiac Failure
Framingham criteria for diagnosis of congestive heart failure (CHF) require at least 1 major criterion and 2 minor criteria.
Major criteria
- Paroxysmal nocturnal dyspnea
- Neck vein distention
- Rales
- Cardiomegaly
- Acute pulmonary edema
- S3 gallop rhythm
- Increased venous pressure
- Positive hepatojugular reflux.
Minor criteria
- Extremity edema
- Night cough
- Dyspnea on exertion
- Hepatomegaly
- Pleural effusion
- Vital capacity reduced by one-third from normal
- Tachycardia (120 beats/min)
Major or minor criterion
- Weight loss 4.5 kg over 5 days of treatment
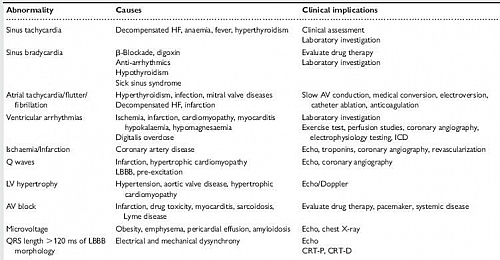
Laboratory Investigations to confirm Heart Failure
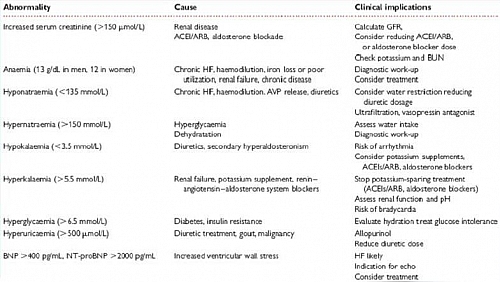
- Full blood count
- Electrolytes, urea and creatinine
- Liver function tests
- Urinalysis
- Blood sugar estimation
- Serum lipid profile
- ECG
- Chest x-ray
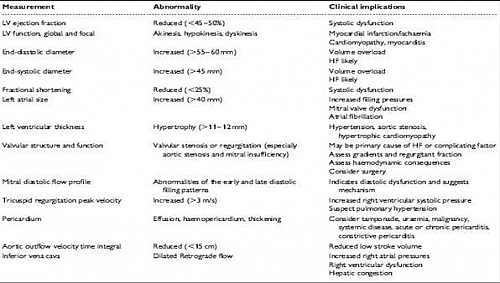
- Echocardiography
- Serum BNP level
- Radionuclide angiography
Differential diagnosis of Heart Failure
- Chronic Kidney Disease (CKD)
- Obesity
- Chronic Obstructive Pulmonary Disease (COPD)
- Nephrotic syndrome
- Chronic Liver Dsiease (CLD)
- Protein losing enteropathies
- Acute severe asthma
- Pulmonary embolism
- Pneumonia
- Shock
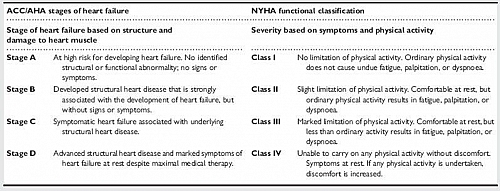
Stages of Heart Failure
- stage A: This is a patient at risk of developing heart failure but no identified structural or functional abnormalities of the heart and also no signs or symptoms of heart failure
- stage B: The patient has developed structural heart disease that is strongly associated with the development of heart failure but without signs or symptoms of heart failure
- stage C: This patient has developed symptoms of heart failure with associated structural heart disease
- stage D: This is advanced structural heart disease and marked symptoms of heart failure at rest despite maximal medical therapy
These stages of heart failure were made by America College of Cardiology (ACC) and American Heart Association (AHA) based on structure and damage to heart muscles.
Classification of Heart Failure
- Class 1: No limitation to physical activity. Ordinary physical activity does not cause undue fatigue, palpitation and dyspnea
- Class 2: Slight limitation to physical activity, comfortable at rest but ordinary physical activity results in fatigue, palpitation and dyspnea.
- Class 3: Marked limitation of physical activity, comfortable at rest, but less than ordinary physical activity results in fatigue, palpitation and dyspnea
- Class 4: Unable to carryon any physical activity without discomfort. Symptoms of heart failure still occurs at rest, if any physical activity is undertaken, discomfort is increased.
This is the New York Heart Association (NYHA) classification of Heart Failure based on symptoms and physical activity.
Treatment of Heart Failure
- Non-pharmacological (i.e. lifestyle modification)
- Pharmacological: drugs which affect preload, myocardial contractility, and afterload
When a treatable underlying cause of congestive heart failure exists, correcting the cause may resolve, or at least greatly improve, the degree of heart failure.
Functions of the Drugs for treatment of Heart Failure
- Digitalis-strengthen the hearts contractions increasing blood flow
- Diuretic-increase the output of salt and water in urine
- Vasodilators-relax blood vessels which lowers the resistance to blood flow. More blood reaches the tissues and the heart works no harder than before.
Non-Pharmacological Treatment of Heart Failure
- Lifestyle modifications
- Patient education on what is heart failure
- Dietary modifications i.e. low salt intake, more vegetables
- Weight reduction in patients with obesity
- Exercise
- Cessation of smoking
- Reduction/cessation of alcohol consumption
List of Drugs for Heart failure treatment (Pharmacological treatment of Congestive Cardiac Failure)
- Diuretics such as Furosemide, Bumetanide
- Angiotensin Converting Enzymes Inhibitors (ACEIs) such as Enalapril, Lisinopril and Captopril
- Angiotensin Receptor Blockers (ARBs) such as Losartan
- Beta blockers such as Carvedilol and Bisoproplol
- Alpha antagonists such as Prazosin
- Direct acting vasodilators such as Hydralazine
- Aldosterone antagonists such as spironolactone
- Cardiac glycosides such as Digoxin
- Anticoagulants
- Anti-arrhythmic drugs such as Amiodarone
Non-pharmacological treatment of Congestive Heart Failure
- Revascularization
- Implantable cardiac defibrillators
- Cardiac transplant
Valve Surgery
If a defective heart valve is responsible for heart failure, it may be treated by heart valve surgery
Angioplasty
Angioplasty, which is catheterization using a balloon to flatten fatty deposits, can be used to treat atherosclerosis or other conditions with blocked arteries.
An artery of an arm or leg is used to guide the catheter through to the blocked artery. An uninflated balloon on the top of a smaller tube is threaded through the larger tube and centered in the plaque narrowed area.
The balloon inflates compressing the plaque against the walls and increasing the open area.
Complications of Congestive Heart Failure
- Deep Venous Thrombosis (DVT)/Pulmonary Embolism (PE)
- Refractory failure
- Multiple organ failure
- Death
Prognosis of Heart Failure
Once Heart Failure becomes symptomatic, it has 2 year mortality rate of 35%, 6 year mortality rate of 80% in men and 65% in women.
50% survive 1 year after pulmonary edema. If cardiogenic shock occurs, up to 85% die after 1 week.
Annual mortality rate depends on patients symptoms and Left Ventricular function: 5% mortality rate in patients with mild symptoms and mild Left Ventricular function and 30% to 50% in patient with advance Left Ventricular dysfunction and severe symptoms.