Table of Contents
- What is Preeclampsia?
- Preeclampsia Blood Pressure Values
- What causes Preeclampsia (Risk factors for Preeclampsia)
- Pathophysiology of Preeclampsia
- Redmans Classification of Preeclampsia
- Types of Preeclampsia based on severity
- Preeclampsia Symptoms
- Signs of Preeclampsia
- Early signs of Preeclampsia
- Management of Preeclampsia (Guidelines)
- Laboratory Investigations in Preeclampsia
- Preeclampsia Treatment
What is Preeclampsia?
Preeclampsia is a multisystem disease that occurs after 20 weeks gestation and is characterized by hypertension and proteinuria with or without edema. It affects many systems of the body. Preeclampsia is a condition of unknown etiology and occurs chiefly in women that are pregnant for the first time (primigravidae); it presents usually in the second half of pregnancy. Although the etiology remains unclear the trophoblast is causative since the condition may be seen before 20 weeks in conditions such as multiple pregnancy or hydatidiform mole, and it is cured by delivery.
Preeclampsia Blood Pressure Values
- A woman has Preeclampsia when she has a blood pressure of 140/90 mmHg or greater in the second half of pregnancy if she was normotensive before this;
- Or when there is a rise of 25 mmHg over the diastolic level in the non-pregnant state or in the first half of pregnancy. This means her blood pressure level before pregnancy or during the early stage of pregnancy (first 20 weeks) must be known if a 25mmHg rise occur above the previous levels, she is said to have Preeclampsia
What causes Preeclampsia (Risk factors for Preeclampsia)
- Primigravid patients
- First pregnancy with a different male partner
- Increased risk with age
- Family history of pre-eclampsia or hypertension
- Pre-existing hypertension, especially renal disease or connective tissue disorder
- Multiple pregnancy
- Diabetic pregnancy
- Hydatidiform mole
- Severe rhesus sensitization
Pathophysiology of Preeclampsia
In normal pregnancy the trophoblast invades the maternal spiral arteries and converts these vessels into low resistance arteries thereby increasing perfusion; in pre-eclampsia this process is defective. Clinically there is evidence of widespread systemic disturbance affecting systems such as the cardiovascular, Hepato-renal system, Central nervous system and the clotting pathway.
It affects the Cardiovascular system by reducing the normal expansion of plasma volume in pregnancy and there may also be a fall in plasma proteins due to renal dysfunction leading to a state of hypovolemia and tissue edema.
The renal system is affected from glomerular and tubular dysfunction. This is detected by the presence of protein in the urine and raised plasma urate levels: Proteinuria greater than 300 mg per volume in a 24 hour collection and Plasma urate greater than 0.35 mmol/litre. Urea and creatinine levels may also rise (levels of greater than 6 mmol/litre and 100 micromoles per litre respectively are significant).
Clotting system is affected in preeclampsia by a falling platelet count and changes in many clotting factors. In severe preeclampsia, there may be progression to disseminated intravascular coagulation (DIC) with micro-angiopathic hemolysis secondary to small vessel blockage, revealed by anemia and the presence of fragmented red cells in the peripheral blood. Raised levels of fibrin degradation products are found.
There could be Liver damage seen as subcapsular haemorrhage and areas of necrosis in the peri-portal region of the liver lobules. Epigastric tenderness has always been described as a sign of impending Eclampsia this has reduced in recent times as awareness of the risk of liver damage has increased and evidence of this damage in the form of elevated enzymes in the mother’s circulation can easily be detected in Liver function tests. The term HELLP syndrome (Haemolysis, Elevated Liver enzymes,Low Platelets) has been formed to emphasize the dangerous combination of disseminated intravascular coagulation and liver damage in severe pre-eclampsia.
In the CNS, there are specific early signs that indicate progression towards Eclampsia such as headache and visual disturbances.
Redmans Classification of Preeclampsia
- Grade 1: Presence of hypertension with no biochemical, hematological and neurological derangement and no symptoms.
- Grade 2: Presence of Hypertension with biochemical derangement (such as hypernatremia, hyperuricemia, elevated liver enzymes and increased TNF) but no hematological, no neurological derangement and no symptoms
- Grade 3A: Presence of Hypertension + Biochemical derangement + Hematological derangement (such as Anemia and thrombocytopenia) and Symptoms but no neurological derangement.
- Grade 3B: Grade 3A + Neurological derangements (such as ankle clonus, hyperreflexia, and brisk tendon reflex)
- Grade 4: Eclampsia
Types of Preeclampsia based on severity
- Significant Proteinuria: proteinuria of 2+ or more on dipstick on two occasions; or > 300mg/day in a 24 hr urine sample; or 1+ with PH < 8 and Specific gravity <1.030 on two occasions
- Mild Preeclampsia: Blood pressure of 140/90mmHg to less than or equals 160/110mmHg on two occasions
- Severe Preeclampsia: BP of greater than 160/110mmHg on two readings or a single reading of 180/120mmHg
Severe Preeclampsia
Severe preeclampsia could be assess based on BP, Urinalysis or Clinical signs. The presence of any of the signs and symptoms mentioned below qualifies for severe preeclampsia.
Signs and Symptoms of Severe Preeclampsia
- Proteinuria of 3+
- Blood pressure: Systolic above 140mmHg or Diastolic above 110mmHg
- Sudden gain of weight within a short period of time
- Epigastric pain, blurring of vision or severe frontal headache
Preeclampsia Symptoms
- Headache
- Visual disturbance
- Abdominal pain
Signs of Preeclampsia
- Sudden weight gain
- Generalized Swelling of the body where signs such as the ring signs and pinard signs are seen. Ring sign (when the woman removes her wedding ring, a depression is seen round the ring finger) Pinard sign (after using the Pinard stethoscope, there would be a ring formed on the abdomen of the woman as a result of the rim of the Pinard stethoscope, this is due to the edema)
- Proteinuria on urinalysis
- Elevated blood pressure above 140/90mmHg
- Headache
Early signs of Preeclampsia
- Urinalysis showing proteinuria in a pregnant woman who is pregnant for the first time and who has passed 20 weeks gestation
- Persistent headache
- Blurring of vision or other visual disturbances
- Epigastric pain (Chest pain)
Management of Preeclampsia (Guidelines)
- Prevention and control of convulsion
- Control of hypertension
- Fluid balance
- Delivery
- Prevention of disseminated intravascular coagulopathy (DIC)
Laboratory Investigations in Preeclampsia
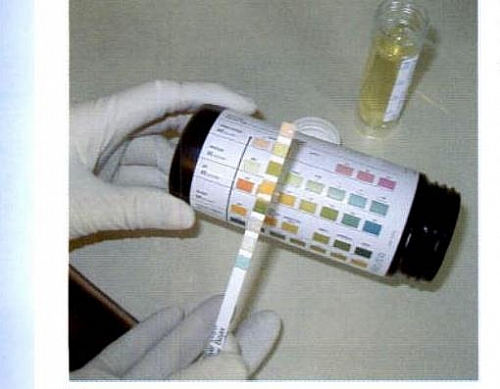
- Urinalysis especially protein content; others are specific gravity, glucose and PH
- Full blood count (FBC) shows elevated Packed cell volume (PCV) and elevated Platelets
- Liver function test shows raised liver enzymes
- Electrolyte, Urea and Creatinine + Uric acid levels
- Clotting profile and Bed side clotting time
- Ultrasound scan for fetal biophysical profile
Preeclampsia Treatment
- Prevention and control of Convulsion: Magnesium sulphate (MgSO4) reduces the risk of eclampsia by around half in women with preeclampsia before delivery or presenting within 24 hours of giving birth. There is a loading dose and maintenance dose using the Pritchard regimen of MgSO4. The loading dose uses 4g of MgSO4 given slowly over 15minutes intravenously when diluted and 10g given intramuscularly into two buttocks (5g each buttock). This helps to prevent convulsions (the more the convulsions, the worse the prognosis. Diazepam could also be used but is not as effective as MgSO4.
- Control of Hypertension: 5mg of Hydralazine given intravenously, slowly over 15 minutes and repeated to a maximum cumulative dose of 20 mg is the approach of choice in the control of hypertension. Other drugs for control of hypertension could be Nifedipine or an infusion of Labetalol. The aim is to reduce diastolic BP to < 100 mmHg.
- Fluid balance: Fluid overload can readily occur and pulmonary edema rapidly develop, therefore standard fluid regimes should be used and monitored.
- Delivery of the Fetus: If the condition is one of severe pre-eclampsia then the timing of delivery will depend on the rate of deterioration of the mother’s condition and the maturity of the pregnancy. Dexamethasone can be given to help in lung maturity before delivery of the fetus (48hours required for maximal effect). If an eclamptic fit has occurred but the baby is alive and viable, delivery should be expedited, often by caesarean section. If the cervix is favorable then induction of labour still has a role, particularly in parous women.
- Depending on the coagulation status of the patient, consideration should be given to prophylaxis of deep venous thrombosis (DVT) and even during the assessment period compression stockings should be provided.