Table of Contents
- Induction of Labour Definition
- When to induce Labour
- Medical Reasons for Induction of Labor (Why do Doctors induce Labor)
- Contraindications of Induction (When not to induce Labour)
- Induction of Labour Methods (Different Ways to bring on Labour)
- How to Induce Labor (Labor Induction Process)
- Induced Labor Risks (Induction of Labour Complications)
- How long does induced labor take?
Induction of Labour Definition
Induction of Labour (IOL) is the initiation of uterine contractions in a woman with intact membrane after the age of viability (28th week of gestation) and before the onset of natural labour by medical and/or surgical means with the sole purpose of achieving a vaginal delivery.
When to induce Labour
Labor can be induced any time from the age of viability which starts from 28 weeks of gestation. The indication for induction of labour may be due to maternal or fetal reasons. It depends on the potential risks or benefits to the fetus and the mother in continuing the pregnancy or terminating it by delivery.
Induction of labour is therefore carried out to deliver a baby that is potentially at risk who is better managed outside the uterus or to improve maternal survival in those women that may be at risk of being harmed as a result of any condition in pregnancy.
Take note that once induction of labour is commenced, there is the potential risk of ending with a caesarean section. Therefore pelvic adequacy, underlying maternal and fetal conditions must be thoroughly evaluated before embarking on IOL. There could be many reasons why Doctors may decide to induce labor and these reasons are listed below under indications for labor induction.
Medical Reasons for Induction of Labor (Why do Doctors induce Labor)
Doctors induce labor due to maternal factors or Fetal Factors, therefore there are Maternal indications and Fetal indications for induction of labour.
Fetal indications for Induction of Labour
- Post term babies (Prolonged pregnancy) babies that are post- date, who have passed the date of normal gestation need to be delivered.
- Intrauterine Growth Restriction (IUGR) when a baby stops growing in the womb, there is need to induce labour else the baby may die
- Previous intrauterine death at term: if there was history of previous death of a baby in the womb at term, then there is need to induce labour in current pregnancy at an earlier age of gestation to avoid intrauterine fetal death (IUFD)
- Rhesus isoimmunisation this happens when the antibodies of the mother begin to attack the baby because the babies blood has sensitized the mothers immune system. This happens when the mothers blood group is Rhesus D negative but the babies blood group is Rhesus D positive.
- Unstable lie
- Fetal death: once there is fetal death, there is no need keeping the pregnancy.
- Fetal abnormality: especially abnormalities that are not compatible with life necessitate induction of labour.
Maternal Indications for Induction of Labour
- Pre-eclampsia: hypertension with significant proteinuria in pregnancy. This is a severe disease that affects both the mother and fetus and the solution is to deliver the baby because preeclampsia is a progressive disease that only worsens and does not regress.
- Eclampsia: when pre-eclampsia occurs with convulsion. Once there is convulsion with proteinuria and hypertension, the baby should be delivered through the fastest possible means after the mother is stable.
- Abruptio placentae: this is the separation of the placenta from the uterus. If the baby is not delivered immediately, there could be intrauterine fetal death.
- Spontaneous or premature rupture of membranes at Term: the rupture of the membranes before 37 weeks of gestation. This leads to infection with several fetal abnormalities.
- Chorioamnionitis: Infection of the chorionic and amniotic membranes
- Polyhydramnios: excessive amniotic fluid
- haemoglobinopathies
- Diabetic mellitus
- Chronic hypertension
- Renal disease
Contraindications of Induction (When not to induce Labour)
- Cephalopelvic disproportion (CPD): when the size of the fetal head cannot pass through the maternal pelvis for whatever reason
- Previous myomectomy where the endometrium was breached
- Placenta previa low lying placenta should not be an indication for induction because the woman may bleed to death
- Active genital herpes: presence of active genital herpes is an indication for C-section and not vaginal delivery
- Malpresentation of the fetus ( such as shoulder, footling, breech, transverse lie)
- Invasive carcinoma of the cervix
- Previous uterine rupture
- Maternal heart disease (NYHA Class III or IV)
- Two or more lower segment caesarean section
- One classical caesarean section.
- Previous Vesico-Vaginal Fistula (VVF) or Recto-Vaginal Fistula (RVF) repair
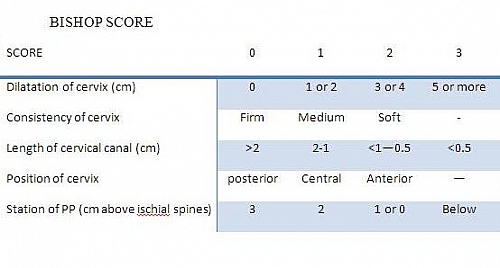
All women undergoing induction of labour should be assessed vaginally for the suitability or favourability of the cervix using the Bishops score.
Induction of Labour Methods (Different Ways to bring on Labour)
- Surgical Methods of Labour Induction – This is done by Amniotomy using the Amniohook or Kochers forceps or the Alligators Forceps. This is simply the artificial rupture of membranes (ARM)
- Medical Methods for Induction of Labour – Oxytocin infusion; use of Misoprostol (which is a prostaglandin E2 analogue and is given as 25 microgram 6 hourly); others are use of Prostglandins E2 (PGE2) and Prostaglandin F2a (PGF2a)
- Mechanical methods such as use of Foleys catheter, sweeping of membranes with gloved finger and extra-amniotic saline infusion
- Unconventional methods of labour induction such as natural methods, use of Acupuncture and homeopathicmethods
How to Induce Labor (Labor Induction Process)
The process for induction of labour involves 2 factors: there should be Strong Uterine contractions and a favorable cervix. When there are no contractions, labour cannot occur and when there are contractions without dilation and softening of the cervix, then there will be complications in labour such as cervical tear or trauma leading to severe bleeding.
Strong Contractions in the induction of Labour
For labour to take place, the uterus is expected to contract strongly in order to push the baby out of the womb. When it contracts strongly, it can achieve this, but when the contractions are weak or moderate, there will be prolong labour with associated complications. In order to avoid prolong labour when there are weak uterine contractions, the labour is sometimes augmented using drugs called Oxytocics and the process is called Augmentation of Labour; an oxytocic helps to increase uterine contractions and makes the contractions stronger. The commonly used oxytocic is Oxytocin. Uterinecontraction is saidto be strong when there are 3 contractions in 10 minutes with each lasting for 45 seconds to 55 seconds. Above 55 secs. gives rise to hyperstimulation and there is risk of uterine rupture.
Favorable Cervix in the induction of labour
Another factor that needs to be considered before induction of labour is how favorable is the cervix to allow the passage of the baby during labor. A favorable cervix needs to be soft, fully dilated, 100% effaced and anteriorly placed. When these criteria are made, delivery will be successful when the woman is induced. The process of making the cervix favorable is called Cervical Ripening.
The cervix can be ripened using different methods and you can know if the cervix is favorable for vaginal delivery to take place by using the Bishops Score. The Bishops score uses 5 parameters and has a score of 0 to 13. A score of 9 and above shows the cervix highly favors vaginal delivery. The Bishops score Table can be seen below
Interpretation of Bishops Score for induction of Labour
- A score of 0-4 means the Cervix is unfavourable (associated with failure, prolonged labour and a high incidence of caesarean section)
- A score of 5-8 means the Cervix is moderately favourable
- A score of 9-13 means the Cervix is ripe and is predictive of successful induction of labour
Methods of Cervical Ripening
- Use of Prostaglandins: agents such as Prostaglandin E2 and Misoprostol are used
- Use of Cervical Dilators such as Intracervical-extra amniotic Foleys catheter, Laminaria tents, Dilapan and Osmotic dilators.
- Sweeping of Membranes using your finger with sterile gloves. This causes the release of prostaglandin
Natural Ways to Induce Labour ( How to Induce Labor Naturally)
- Encouraging sexual intercourse with your husband
- Nipple stimulation
- Use of castor oil
Induced Labor Risks (Induction of Labour Complications)
- Fetal distress
- Iatrogenic prematurity
- Uterine rupture
- Failed induction leading to caesarean section with associated complications
- Fetal hyperbilirubinemia
How long does induced labor take?
Once you induced a woman, delivery should occur within 12 hours and should not exceed this time. Induction of labour does not mean you will deliver quickly; once a woman is induced, the process continues just a normal labour and there may be need to augment the labour and sometimes even caesarean section may be the last resort. Therefore, making sure the cervix is ripe, the contractions are strong and that there is no fetal distress nor maternal problems during the process is the key to a successful induction of labour.