Schistosoma haematobium is a blood fluke that causes a type of schistosomiasis known as Urinary Schistosomiasis because it affects the urinary tract and capable of causing bladder cancer. Schistosoma haematobium infection has an incubation period of 10 to 12 weeks or longer with morbidity rate as high as 50 to 70%. Schistosoma haematobium is the commonest of the different species of schistosoma and has been known for over 3000 years in Egypt which has the world’s highest incidence.
Table of Contents
- Schistosoma haematobium Epidemiology
- Schistosoma haematobium Transmission
- Schistosoma Haematobium Egg (Ova)
- Schistosoma Haematobium Morphology and Characteristics
- Life cycle of Schistosoma Haematobium
- Schistosoma Haematobium Pathogenesis
- Schistosoma Haematobium Symptoms and Signs
- Schistosoma Haematobium Diagnosis
- Schistosoma Haematobium Treatment
- Schistosoma haematobium Complications
- Schistosoma haematobium Prevention
Schistosoma haematobium Epidemiology
Schistosoma haematobium disease is endemic in some parts of Africa such as Egypt, Israel, Syria, Saudi Arabia, Iran, Iraq and the shores of Chinas great lakes. Freshwater snails of the genus Bulinus (e.g. Bulinus truncatus) serve as the intermediate host for schistosoma haematobium.
Schistosoma haematobium Transmission
The mode of transmission of Schistosoma haematobium occurs through contact with water containing free swimming larvae called cercariae (the infective stage of schistosoma). When the skin is exposed to the bifid-tailed embryos (cercariae) of the trematode Schistosoma, they penetrate the skin and shed their tails and are then taken via the blood to other parts of the body.
Schistosoma Haematobium Egg (Ova)
S. haematobium eggs are ovoid in shape with a terminal spine. The egg measures about 83-187 micrometers by 60-70 micrometers and can be seen in urine or stool when viewed with a microscope. At the site of their deposition, the eggs lie in chainlike rows within small veins.
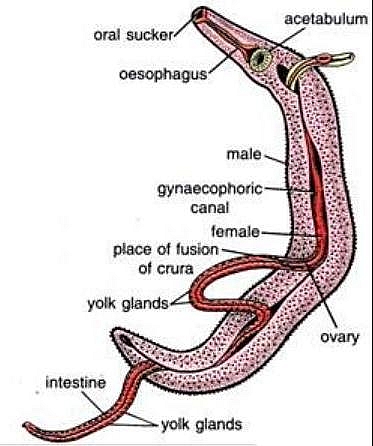
Schistosoma Haematobium Morphology and Characteristics
- The egg of schistosoma haematobium is ovoid in shape and can be distinguished by the terminal spine
- The male adult worms measure 715mm in length while the females measure 920 mm
- The adult male worms are thicker than the females
- Even though the female adult worms are longer than the males, the females often coil up in a tegumental fold known as the ventral groove or canalis gynaecophorus
- A characteristic feature of the approximately 340520 micrometer long cercariae is their forked tail
- Adult worms reside in the Venous plexus of minor pelvis of the kidney
Life cycle of Schistosoma Haematobium
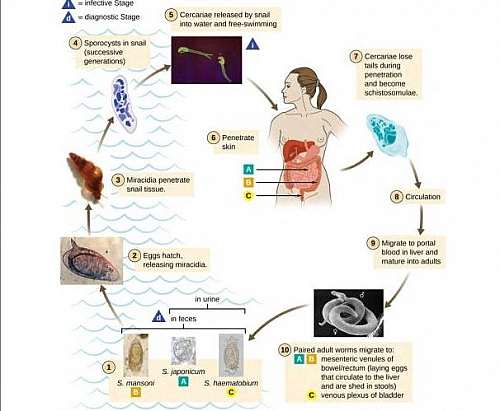
- Hundreds of schistosoma haematobium eggs are released daily by adult worms in stool
- The released eggs then hatch into immature ciliated larvae called Miracidia freshwater
- Miracidia then penetrates Bulinus snails in freshwater within 36 hours or they die
- In the snails liver, the miracidium enlarges and gives rise to myriads of daughter cysts which are released after the snail dies
- Sporocysts now develop into mature larvae called Cercariae which is infective stage of Schistosoma
- Cercariae can now penetrate the human skin to cause Schistosomiasis. When in the body tissue, cercariae lose their tails to become Schistosomutae.
- After shedding their tails, they enter blood vessels and are carried to all parts of the body but they flourish in the liver where they live on erythrocytes and develop into male and female worms.
- After attaining sexual maturity in the liver, the nematodes now leave the liver and enter the portal vein
- Schistosoma haematobium has an affinity for the Bladder venous plexus, which it reaches through the portosystemic anastomotic channels
- When the worms reach the bladder, the female worm eventually enters a submucous venule which is so small that she completely blocks it and starts laying ova in a chain; each ovum is provided with a terminal spine that penetrates the vessel wall
- The life cycle of schistosoma haematobium is completed when the eggs become released into stool or urine
Schistosoma Haematobium Pathogenesis
Majority of the symptoms and signs of Schistosoma haematobium infection are caused by passage of the eggs through the mucosa of the urinary tract causing granulomatous reaction as a result of deposition of Schistosoma haematobium eggs in tissues especially the bladder and leading to sandy patches and microgranulomas; S. haematobium can cause obstruction of the ureteric orifices resulting in obstructive uropathy.
Metastatic Schistosomiasis
In some rare cases schistosoma haematobium eggs may be carried to other parts of the body apart from the bladder this is known as Metastatic schistosomiasis. When the eggs are in the central nervous system , the CNS (brain, spinal cord) they cause Cerebral Schistosomiasis by compressing the spinal cord and causing acute paraplegia. When the eggs are in the lungs, they cause Pulmonary schistosomiasis by triggering fibrous reaction leading to pulmonary fibrosis and pulmonary hypertension. Other organs can also be affected such as endocrine organs and gonads.
Schistosoma Haematobium Symptoms and Signs
Symptoms and signs result from the ova of schistosoma because the eggs release antigenic substances that trigger immune response. They symptoms include early and late symptoms.
Early Symptoms of Schistosoma haematobium infection (Katayama Syndrome)
- Itching at the site of penetration of cercariae for about 1 to 2 days followed by Katayama Fever 3 to 5 weeks after itching
- Urticaria
- Eosinophilia
- Fever
- Muscle aches
- Abdominal pain
- Splenomegaly
- Headache
- Cough
- Sweating
Clinical Features of established Schistosoma haematobium disease
- Painless terminal hematuria (especially in children) while other complications occur in adults. The hematuria is intermittent and usually occurs after strenuous exercise and is found in about50% of patients
- Groin pain
- Frequency of micturition (Urinating frequently)
- Features of upper urinary tract dilatation from obstruction of the ureteric orifices
- There may be pyelonephritis that could lead to hypertension and uremia
Schistosoma Haematobium Diagnosis
- Diagnosis of Schistosoma haematobium occurs by identification of Schistosoma haematobium egg in urine or in stool using a light microscope
- Rectal snip for Schistosoma haematobium ova
- Urea, Electrolyte and Creatinine levels to check for renal status
- Cystoscopy may show typical urinary bladder lesions such as bladder wall fibrosis and calcifications
- Bladder biopsy and histology demonstrates ova in biopsy sample
- Abdominal Ultrasound scan may show hydroureters and hydronephrosis
- Intravenous Urogram may reveal contracted bladder
Schistosoma Haematobium Treatment
- The drug of choice for the treatment of Schistosoma haematobium is Praziquantel. Using a dose of 40mg/kg stat and it is repeated after 3 weeks for all stages of Schistosomiasis caused by schistosoma haematobium.
- Metrifonate is an alternative drug that is effective against S. haematobium and given in dosage of 7.5 10mg/kg in 3 doses at 2 weeks interval
- Surgery to correct bladder abnormalities
- Renal replacement therapy if End Stage Renal Disease (ESRD) develops
Schistosoma haematobium Complications
- Painless terminal hematuria in Children the blood is observed at the end of urination
- Bladder cancer
- Calcifications in the urinary Bladder wall
- Fibrosis of the bladder wall due to secondary infection
- Pyelonephrosis
- Hydronephrosis
- Urethral strictures
- Bilharzial pseudotubercles the earliest specific sign of schistosoma haematobium to appear that can be detected through cystoscopy.
- Bilharzial nodules these develop by the fusion of tubercles
- Sandy patches that occur as a result of calcified dead ova with degeneration of the overlying epithelium
- Ulceration is the result of sloughing of the mucous membrane of the bladder containing dead ova
- Granulomas (Bilharzial masses) – caused by the aggregation of nodules
- Papillomas these are more pedunculated
Schistosoma haematobium Prevention
- Regular drug therapy of specific population groups
- Elimination of snails populations in freshwater bodies
- Provision of safe and adequate water
- Environmental hygiene to avoid improper disposal of human feces
- Avoidance of skin contact with natural or artificial bodies of water (freshwater)