Table of Contents
- Hyperemesis gravidarum Meaning
- Hyperemesis gravidarum Definition
- Hyperemesis Gravidarum Incidence
- Hyperemesis gravidarum Causes and Risk Factors (Etiology of Hyperemesis gravidarum)
- Hyperemesis gravidarum Symptoms and Signs
- Laboratory investigations in Hyperemesis gravidarum
- Management of Hyperemesis gravidarum
- Hyperemesis gravidarum Treatment
- Hyperemesis gravidarum Complications
- Hyperemesis gravidarum Differential diagnosis
Hyperemesis gravidarum Meaning
Hyperemesis gravidarum (also called Pernicious vomiting of pregnancy) is the medical term for severe morning sickness. It is a severe form of Nausea and vomiting in early pregnancy that requires hospitalization. Hyperemesis gravidarum is an intractable vomiting seen in a pregnant woman that leads to fluid and electrolyte disturbances and nutritional deficiencies. Occasionally there is a progression from ordinary nausea and vomiting to the rejection of all kinds of food and drink. If uncheck, this disease may lead to dehydration and starvation with ketosis, liver damage, jaundice, neuropathies and even death.
Hyperemesis gravidarum Definition
Hyperemesis gravidarum is a severe disease in early pregnancy that causes excessive nausea and vomiting probably due to the effects of large amounts of circulating steroids, especially estrogens or HCG and seldom last beyond the 16th week of pregnancy. Hyperemesis gravidarum may occur at any time of the day and is aggravated by cooking and fatigue. Mild cases (often referred to as Morning Sickness) are treated by a light carbohydrate diet (biscuits and milk) in the morning and sometimes by anti-emetics.
Hyperemesis Gravidarum Incidence
Incidence of hyperemesis gravidarum worldwide is < 0.5 to 2%. Incidence in the United Kingdom is less than 1:1000 pregnancies.
Hyperemesis gravidarum Causes and Risk Factors (Etiology of Hyperemesis gravidarum)
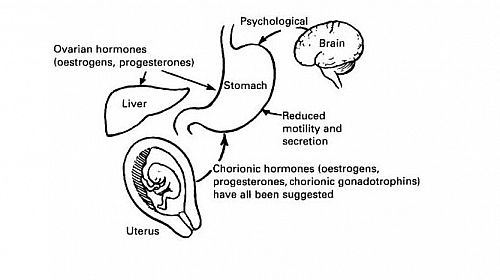
- Hormonal causes: such as rapid increase in hCG levels in the blood (stimulating Chemoreceptor trigger zone in the brain) and also increase in progesterone level. Hypothyroidism could also cause Hyperemesis gravidarum.
- Ketosis: Hyperemesis gravidarum becomes excessive and forms a vicious circle due to build-up of ketones that further exacerbates the vomiting
- Hydatidiform mole: the presence of Hydatidiform mole that mimics pregnancy by producing excessive amounts of hCG leads to hyperemesis gravidarum.
- Psychological cause: the fear of pregnancy or fear labour could trigger hyperemesis gravidarum
- Allergy to corpus luteum
- Multiple pregnancy: having twins or triplets or more increases the production of hCG and therefore there will likely be hyperemesis gravidarum
- Dietary deficiency: such as deficiency of vitamin B1 and Vitamin B6
- Hepatic and gastric dysfunction
Hyperemesis gravidarum Symptoms and Signs
- Vomiting that contains bile (looks yellowish green) and tastes bitter. Vomitus may also be blood stained from retching. Usually the vomiting starts at 1st month of pregnancy and resolves by the end of the 1st trimester of pregnancy (end of 1st three months of pregnancy).
- Weight loss because of loss of body fluid and burning up of fat
- Haemoconcentration and unstable acidbase balance
- Ketosis
- Thirst
- Oliguria passage of small volume of urine
- Features of Wernickes encephalopathy such as drowsiness, nystagmus, loss of vision and coma.
- Other signs include features of dehydration such as loss of skin elasticity, sunken eye balls, dry tongue, rapid and weak pulse, and low blood pressure
Laboratory investigations in Hyperemesis gravidarum
Some lab tests are required to help in treatment of hyperemesis gravidarum and to rule out other possible causes of vomiting in pregnancy. These laboratory tests are mentioned below with their reasons.
- Full blood count with differentials: to rule out infections
- Blood film and microscopy to rule out malaria in pregnancy
- Urinalysis and Urine M/C/S to rule out Urinary tract infections (UTI)
- E/U/Cr to assess electrolyte derangement
- Abdominopelvic ultrasound scan to rule out molar pregnancy, multiple pregnancy, ovarian torsion and also to date pregnancy and confirm fetal viability.
- Liver function tests (LFTs) to rule out liver involvement such as fatty infiltration from chronic starvation.
- Random blood sugar to rule out hypoglycemia (low sugar levels in the blood)
Management of Hyperemesis gravidarum
There are other diseases that may mimic the symptoms of hyperemesis gravidarum and there is need to exclude these diseases such as Urinary infection, Hiatus hernia and gall bladder disease, Obstructive gut lesions, and Central nervous system (CNS)-expanding lesions.
There is need to also exclude obstetric causes such as Multiple pregnancy, Hydatidiform mole and acute yellow atrophy of the liver.
Hyperemesis gravidarum Treatment
- Restore fluid and replace calorie with 5% Dextrose saline or dextrose water
- Electrolyte correction using Normal saline, Ringers lactate or Potassium supplement (if there is demonstrable Hypokalemia)
- Use of antiemetics such as I.M promethazine (25mg, 8 hourly for 24 hours), other drugs that could stop the vomiting include Cyclizine or Metoclopramide (Maxolon).
- Supplements of Thiamine to prevent Wernickes encephalopathy
- Steroid therapy: some severe cases may respond to steroid therapy or odansetron
- Psychological treatment such as psychological support or counseling as most patients respond to suggestion. If not, formal psychotherapy is needed.
- Therapeutic abortion very rarely required.
Hyperemesis gravidarum Complications
- Dehydration
- Hypovolemia that could cause Hypovolemic shock
- Acute renal failure (ARF)
- Weight loss
- Electrolyte depletion
- Wernicke-Korsakoff encephalopathy
- Hypoglycemia
- Gastrointestinal mucosa tear such as Mallory-Weiss tear
- Aspiration pneumonitis
- Hepatic dysfunction causing jaundice
- Nutritional deficiencies
- Dental caries
- Vitamin deficiency, particularly thiamine (Vitamin B1)
- Death from liver failure or the end processes of the above
Hyperemesis gravidarum Differential diagnosis
- Urinary tract infections (UTI) in pregnancy
- Malaria in pregnancy
- Acute appendicitis
- Intestinal obstruction and adhesions
- Ovarian torsion
- Gestational trophoblastic disease (GTD)
- Gall bladder disease such as cholecystitis