Table of Contents
What is Leishmaniasis?
A leishmaniasis is a group of parasitic infectious diseases caused by protozoa of the genus Leishmania that is transmitted by the bite of the female phlebotomine sandfly as the vector. This means Leishmaniasis is not just a single disease but a group that has different symptoms and signs depending on the type that a patient may have. The types of Leishmaniasis will be described below.
Causes of Leishmaniasis
It is caused by a parasite of the genus Leishmania –this genus includes four major parasites that cause the different clinical types. These 4 major parasites include Leishmania donovani, Leishmania tropica, Leishmania mexicana, and Leishmania braziliensis.
Mode of Transmission
Leishmaniasis is transmitted by the bite of an infected female phlebotomine Sandfly – which is the vector while mammals serve as the reservoirs of the parasite such as dogs, rodents (rodents are the major reservoirs in East Africa, Ethiopia, Sudan, and Kenya), and foxes (canines are the major reservoirs in the Mediterranean and Asia); in some species of Leishmania parasite, man is the reservoir. Only the female sand flies transmit Leishmaniasis because they need a blood meal as a requirement for the maturation of their eggs.
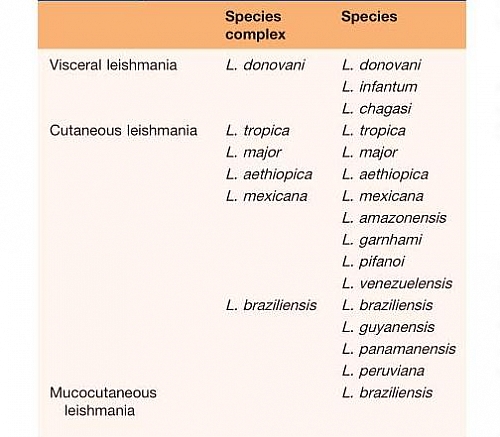
Clinical forms (Types of Leishmaniasis)
- Visceral Leishmaniasis
- Cutaneous Leishmaniasis– which may consist of Simple cutaneous lesions or Diffuse cutaneous lesions
- Mucocutaneous Leishmaniasis
The above classification refers to the broad classification of Leishmaniasis based on the areas of the body affected. Each of the broad types has subtypes that are grouped based on the species of organisms causing it and will be discussed in detail in each of the types of clinical leishmaniasis.
Leishmania Life cycle
- The leishmania life cycle starts when an infected female sandfly takes a blood meal from a human host leading to the injection of promastigote forms of the leishmanial parasite into the blood through the proboscis of the sand fly as it feeds.
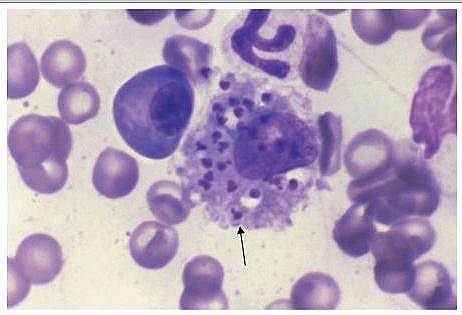
- As the promastigote forms of leishmania species enter the blood, they become ingested by macrophage
- Inside the macrophages, the promastigotes change into non-motile amastigote forms and they start to reproduce by binary fission (division into two) in the macrophages of the reticuloendothelial system consisting of the lymph nodes, liver, bone marrow, and spleen. The amastigotes keep increasing by division until the macrophage cell eventually bursts to release more into the blood which then infects other macrophages again. Even though the macrophages are supposed to destroy these infectious organisms, they fail to do so because the Amastigotes can prevent the fusion of the vacuoles with lysosomes, and hence the macrophage cannot destroy them.
- Whenever another sandfly bites an infected human host, it ingests the amastigotes in the blood which then differentiate into promastigotes in the gut of the female sandfly. The promastigotes then multiply in the gut of the sand fly and migrate to the pharynx, where they can be transmitted during the next bite. The cycle in the sandfly takes approximately 10 days.
- The life cycle is completed when the female sandfly bites a new host and injects the promastigotes into the blood
Epidemiology
The geographical distribution of Leishmaniasis varies and some species of Leishmania parasite are specific to certain areas. Leishmaniasis is commonly seen in Asia (especially in places like India and Bangladesh), Africa, Europe, the Middle East, South America and Central America.
Leishmaniasis Symptoms and Signs
The symptoms of leishmaniasis depend on the type of parasite and also on the host cell-mediated immune response.
- Sometimes, one may be infected but there may be no symptoms (Asymptomatic infection), this is because the parasite is suppressed or eradicated when the individual has a strong immune system. This is common in endemic areas, a positive leishmanin skin test without symptoms shows the individual has been exposed to Leishmaniasis.
- Intermittent fever, weakness, and weight loss with massive enlargement of the spleen (massive splenomegaly) are characteristic typical of Visceral Leishmaniasis (also known as Kala azar, which means black fever or Black sickness due to the hyperpigmentation of the skin caused by visceral Leishmaniasis.
- Symptomatic infection may be confined to the skin in Cutaneous leishmaniasis which presents with symptoms of ulceration of the skin
- Sometimes, the ulceration may spread to the mucous membranes in the case of Mucocutaneous leishmaniasis.
Laboratory Diagnosis
- Specific diagnosis of Visceral Leishmaniasis is made when the Leishmania parasite is seen with a microscope in stained smears of aspirates of lymph node, bone marrow, liver, or spleen; Culture of the specimens from bone marrow, lymph node, liver, and spleen can also be done
- In Cutaneous Leishmaniasis, the parasites can be detected by PCR; a biopsy of the edge of the ulcer can be taken for histology and Giemsa stain on a split-skin smear helps to identify leishmania parasites in 80% of cases
- Specific serological tests are positive in many cases; Leishmanin skin test showing negative may not indicate the absence of Leishmaniasis but may indicate a poor cell-mediated immune response.
- Parasites can also be detected by PCR
The Leishmanin Skin Test
This is a test done to help in the screening of Leishmaniasis. It shows if the patient has been exposed but does not show if the infection is active or not. It is usually done by injecting killed Leishmania parasite into the skin just as it is done in the PPD skin test for tuberculosis; a raised indurated papule on the skin after 48 hours shows there is the presence of Leishmania infection.
Leishmaniasis Treatment
- The widely used drugs for visceral leishmaniasis are the pentavalent antimony salts such as sodium stibogluconate with antimony or meglumine antimonite (commonly used in some countries such as India) resistance to these drugs is increasing.
- The best drug for the treatment of Leishmaniasis is intravenous amphotericin B (even though it is costly)
- Oral Miltefosine has been shown to be highly effective in India
- Secondary bacterial infections are treated with antibiotics
- Blood transfusion may occasionally be required
- Small lesions in cutaneous leishmaniasis usually require no treatment but large lesions or those in cosmetically sensitive sites can sometimes be treated locally, or by curettage or use of cryotherapy or topical anti-parasitic agents
Prevention
- Prevention of Leishmaniasis basically entails control of the vector the sand fly. This can be done by use of nets on windows and beds while sleeping
- Avoid sleeping on the ground in endemic areas as sand flies are poor fliers which helps prevent bites when you don’t sleep on the floor.
- Use of insecticide to kill sand flies
- Prompt treatment of infected humans to prevent transmission of infection to others as humans may serve as reservoirs in some species of Leishmania parasite.