Tuberculosis and HIV/AIDS co infection refers to a condition whereby someone has both TB and HIV together. This co infection is very dangerous as it promotes the progression of both diseases. The Tuberculosis makes it easier for HIV to progress rapidly while the HIV makes it possible for Tuberculosis to spread leading to extrapulmonary TB such as Miliary TB and becomes more complicated; because of this, patients with TB need to be tested for HIV and those with HIV need to be tested for TB with tuberculin skin testing and/or chest x-ray.
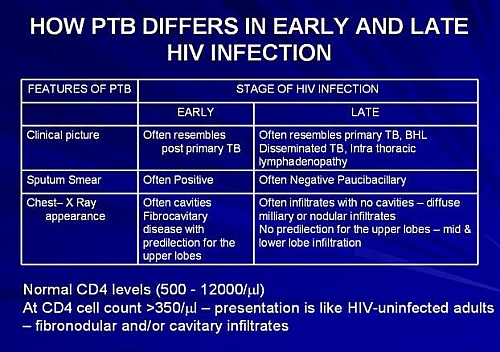
Patients with HIV and a positive tuberculin skin test develop active TB at a rate of 3-16% per year and are more likely to have disseminated disease and less likely to have upper-lobe infiltrates or cavitary pulmonary disease. Patients having HIV and TB co infection with a CD4 count of less than 200 may have mediastinal adenopathy with infiltrates.
Table of Contents
Why HIV/AIDS infected patients are at risk of TB infection
HIV infected patient are at risks for primary or reactivation of TB and for second episode of TB from exogenous re-infection. This susceptibility is related to pattern of cytokines produced by T-lymphocytes. T1 lymphocytes which produce interferon- are central to anti-mycobacterial immune defenses. Fatal mycobacterial disease develops in children who lack interferon- receptors. T2 lymphocytes which produce interleukin 4 and interleukin 10 do not contribute to anti-mycobacterial immunity; the reduced T1 response in HIV infected patient is what contributes to susceptibility to TB.
Management and Treatment Guidelines of HIV and TB co infection
Treatment regimens for active or latent TB in patients with HIV are similar to the treatment of individuals who are HIV negative the standard short course tuberculosis treatment is followed with little differences such as the avoidance of rifampicin in patients who are on ARV with protease inhibitors or non-nucleoside reverse-transcriptase inhibitors (NNRTI) because rifampicin induces activities of cytochrome P-450 CYP3A which reduces the concentration of HIV Protease Inhibitors (PI) and NNRTI to sub therapeutic levels leading to incomplete viral suppression and emergence of drug resistance; hence the concomitant administration of rifampicin with PIs and NNRTI is not recommended.
New anti-retroviral combination regimens have dramatically improved the prognosis for HIV infected patient with TB.
Rifabutin may be used in place of rifampicin in patients who are on indinavir, nelfinavir, or efavirenz because it is a less potent inducer of cytochrome P-450 CYP3A and can therefore be administered in combination with Protease inhibitors such as indinavir or nelfinavir or amprenavir (which is still under development). Rifabutin should not be used with hard gel formulation of saquinavir because of decrease drug levels.
Indinavir can be given in increase dose of 1000 mg every 8 hours in patient receiving rifabutin- this reduces a likelihood of drug resistant HIV mutant. Protease inhibitors inhibit metabolism of rifabutin will increase likelihood of developing uveitis- a reduce dose of rifabutin, 150mg daily is therefore recommended.
Protease inhibitors are recommended as part of initial therapy in patient with more than 5000 copies of HIV RNA per ml.
Thiacetazone should never be used for treatment of TB in HIV patients, since it is associated with increased risk of severe and in some cases fatal skin reactions.
Patients with HIV and TB may develop a paradoxical response when starting antiretroviral therapy (ARV); this response has been attributed to a stronger immune response to Mycobacterium tuberculosis. Such a response is signified by the following symptoms and signs: fever, worsening pulmonary infiltrates, and lymphadenopathy.