Hypospadias is a relatively common congenital defect of the male external genitalia in which the urethra opens at an abnormal position at the under surface of the penile shaft to the perineum.
Table of Contents
- Hypospadias Epidemiology
- What is hypospadias?
- Hypospadias Embryology
- Hypospadias Characteristics on Clinical examination
- Hypospadias Causes (Etiology)
- Hypospadias classification and types based on position of the urethral opening
- Other forms of Classification of Hypospadias
- Hypospadias Symptoms and Signs (Clinical manifestations)
- Hypospadias diagnosis and investigations
- Hypospadias Associated Anomalies or Birth defects
- Hypospadias treatment and Management approach
- Complications of Hypospadias Surgery
- Hypospadias Complications
- Hypospadias differential diagnosis
Hypospadias Epidemiology
Hypospadias is present in approximately 1 in 250 male newborns; it may occur as an isolated defect or may be associated with other congenital defects such as an intersex state (ambiguous genitalia).
What is hypospadias?
Hypospadias is an abnormal ventral opening of the urethral meatus that may be located anywhere from the ventral aspect of the glans penis to the perineum.
Hypospadias Embryology
The Penis and associated urethra develop from 3 structures: the glans develops from the genital tubercle; penile urethra develops from the urethral folds while the scrotum develops from primitive genital swellings.
The urethral folds normally fuse cranio-caudally to form a complete urethra. Hypospadias occurs due to failure of complete fusion of the urethral folds.
Hypospadias Characteristics on Clinical examination
- Ventral urethral opening
- Splayed and flattened glans (spade-like glans)
- Dorsal Hooding
- Chordee: which may be due to Skin tethering
- Presence of fibrous band adjacent to urethra
- Short urethra
- Corporal disproportion
Chordee is not present in all patients having hypospadias
Hypospadias Causes (Etiology)
- Abnormal androgen production by the fetal testis
- Limited androgen sensitivity in the target tissues of the developing external genitalia
- Premature cessation of androgenic stimulation secondary to premature involution of Leydig cells of the fetal testis
- Insufficient testosterone and/or dihydrotestosterone synthesis -presumably defective or deficient 5 alpha-reductase enzyme activity
- Defective androgen receptor quality and/or quantity
- Environmental Endocrine Disruptors
- Hypospadias may be Hereditary in 1 out of 10 cases – which means a child may inherit it if the father had hypospadias as a child
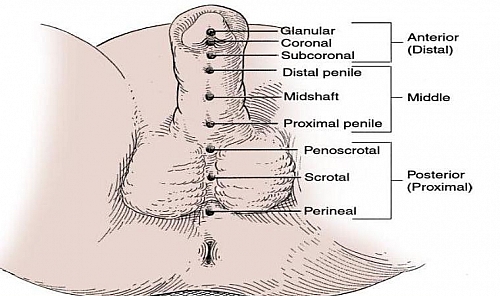
Hypospadias classification and types based on position of the urethral opening
- Glanular Hypospadias: when the urethra opens at the glans
- Coronal Hypospadias: this occurs when the urethra opens below the normal position of the urethral meatus
- Subcoronal Hypospadias: when the urethra opens at the junction of the glans and the shaft
- Distal Penile Hypospadias: when the urethra opens at the shaft but near the glans
- Midshaft Hypospadias: when the urethra opens at the middle of the penile shaft
- Proximal penile Hypospadias: when the urethra opens at the shaft but near the scrotum
- Penoscrotal Hypospadias: when the urethra opens at the junction between the shaft and the testis
- Scrotal Hypospadias: when the urethra opens on the scrotum
- Perineal Hypospadias: when the urethra opens in the perineum
Other forms of Classification of Hypospadias
- Distal or Anterior Hypospadias: this includes the glanular, coronal and subcoronal type of hypospadias
- Middle Hypospadias: this includes the distal penile, midshaft and proximal penile hypospadias
- Proximal or Posterior l Hypospadias: this includes the penoscrotal, scrotal and perineal hypospadias
Hypospadias Symptoms and Signs (Clinical manifestations)
- Abnormal ventral opening of the urethral meatus
- Abnormal distribution of foreskin with a hood present dorsally (dorsal hooding of the penis)
- Abnormal ventral curvature of the penis (Chordee)
The consistent feature of Hypospadias is the ventrally placed abnormal urethral opening. Chordee and hooding may not be present in all cases.
Hypospadias diagnosis and investigations
Diagnosis is clinical and based on the characteristics listed above. Investigations are done to prepare the child for surgery and to exclude other associated anomalies.
- Abdominopelvic ultrasound scan to exclude other associated anomalies an also to exclude cases of ambiguous genitalia
- Urine microscopy, culture and sensitivity to exclude Urinary tract infections (UTI)
- Packed cell volume and Genotype to prepare patient for surgery
Hypospadias Associated Anomalies or Birth defects
- Undescended Testis
- Hernia
- Renal anomaly
- Posterior Urethral Valve (PUV)
- Intersex
Hypospadias treatment and Management approach
Definitive Hypospadias treatment is surgical repair; and this is aimed at achieving normal voiding of urine, for Cosmesis, for normal sexual function and fertility
Best time for Hypospadias Surgery
- Best time is at the age of 6 months to 24 months (2 years) and when circumcision has not been carried out yet. The age of 6 months to 2 years is preferred because there is no added risk of anesthesia after 6 months, there is sufficient development, sexual orientation and parental bonding is less affected and easy to manage post-operatively.
- If phallus is too small, it may be increased by application of Testosterone cream or controlled intramuscular testosterone given monthly for not more than 3 months.
Principles of Hypospadias surgical repair
- Appropriate timing of surgery
- Control of UTI (if present) before surgery
- Use of appropriate instruments and sutures (Fine suture sizes – 6/0, 5/0, 4/0)
- Use of magnification lenses (Loupes)
- Meticulous handling of tissues
- Use of vascularized flaps
- Use of Non-hair bearing skin
Complications of Hypospadias Surgery
- Penile edema
- Wound infection
- Fistula formation
- Complete wound dehiscence
- Urethral stricture
- Urethral meatal stenosis
These complications may arise and good surgical skills with good preoperative and postoperative care will reduce them greatly.
Hypospadias Complications
- Infertility
- Risk of developing recurrent urinary tract infections
Hypospadias differential diagnosis
- Epispadias
- Intersex