Table of Contents
What is Hysterosalpingogram or Hysterosalpingrography?
Hysterosalpingography or Hysterosalpingogram is a radiological procedure that gives information about the uterine cavity and isthmus of the fallopian tube, that laparoscopy and dye cannot provide such as adhesiolysis or ovarian cystectomy. Hysterosalpingograms (HSG) are used in women with no history of pelvic damage or infection.
The test is usually performed during the follicular phase of the menstrual cycle prior to ovulation in order to avoid the risk of inducing an ectopic pregnancy or inadvertently exposing an early embryo to ionizing radiation.
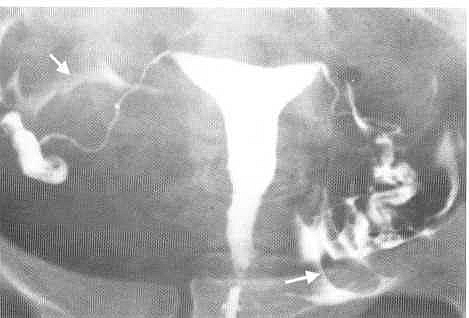
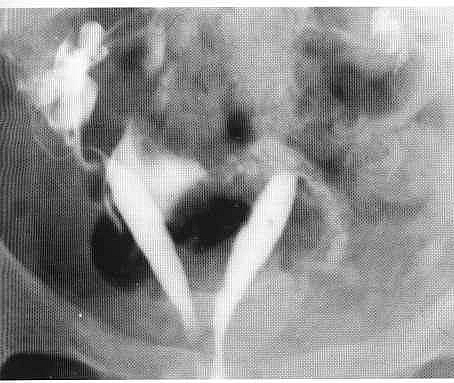
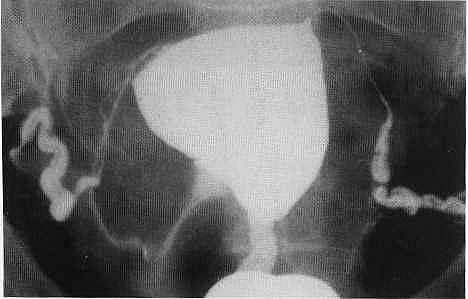
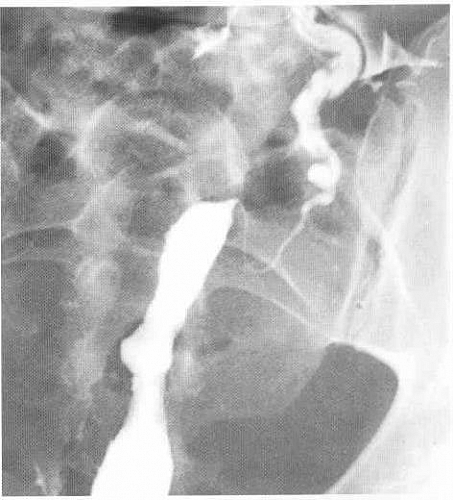
The procedure involves the instillation of a radio-opaque dye, through a small catheter placed in the cervical canal, into the uterine cavity. The X-ray image obtained shows the uterine cavity, the outline of the Fallopian tubes and the presence or absence of dye in the abdominal cavity.When dye is seen to flow freely into the abdominal cavity, tubal patency is confirmed. However, if the dye spill appears to be loculated or the tube appears to be in an abnormal position, peri-tubal adhesions are likely to be present: Uterine adhesions and submucous fibroids appear as filling.Defects on the X-ray image and require further assessment by hysteroscopy.
Indications for Hysterosalpingography (HSG)
- Infertility
- Recurrent miscarriages
- Following tubal surgery
- Assessment of the integrity of a Caesarean uterine scar
Hysterosalpingogram Contraindications
- Pregnancy
- Acute Pelvic Inflammatory Disease (PID)
- Recent dilatation and curettage, abortion or immediately post-menstruation
- Contrast sensitivity
Contrast medium used in HSG
Oily contrast medium is no longer recommended. High Osmolar Contrast Medium (HOCM) or Low Osmolar Contrast Medium (LOCM) can be used at a volume of 10-20 ml.
Equipment used in HSG
- Fluoroscopy unit with spot film device
- Vaginal speculum
- Vulsellum forceps
- Uterine cannula, Leech-Wilkinson cannula, olive or 8-F paediatric Foley catheter.
Patient preparation for HSG
- TEN DAY RULE: The examination can be booked between the fourth and tenth days in a patient with a regular 28-day cycle.
- Apprehensive patients may need premedication.
Preliminary film
Coned Posterior Anterior (PA) view of the pelvic cavity.
Hysterosalpingogram Procedure (Technique)
- The patient lies supine on the table with knees flexed, legs abducted and heels together.
- Using aseptic technique the operator inserts a speculum and cleans the vagina and cervix with chlorhexidine.
- The anterior lip of the cervix is steadied with the vulsellum forceps and the cannula is inserted into the cervical canal.
- Care must be taken to expel all air bubbles from the syringe and cannula as these would otherwise cause confusion in interpretation. Contrast medium is injected slowly under intermittent fluoroscopic control.
- Spasm of the uterine cornu may be relieved by intravenous buscopan or glucagon.
Types of Views taken in Hysterosalpingogram Films
- AP projection as the tubes begins to fill.
- Right anterior oblique
- Left anterior oblique
- Delayed (30 minutes) AP Projection with all the instruments removed.
Aftercare of Hysterosalpingogram
- It must be ensured that the patient is in no serious discomfort nor has significant bleeding before she leaves.
- The patient must be advised that she may have bleeding per vaginam for 1-2 days and pain may persist for up to 2 weeks.
Complications or Side effects of HSG
- Allergic phenomena – especially if contrast medium is forced into the circulation; allergies may occur.
- Pain may occur at the following times: using the vulsellum forceps may hurt, during insertion of the cannula, tubal distension proximal to a block, with distension of the uterus if there is tubal spasm or peritoneal irritation may occur up to 2 weeks. Any of this hurts but can be reduced by a skilled hand.
- Bleeding from trauma to the uterus or cervix.
- Transient nausea, vomiting and headache.
- Infection: This may be delayed and occurs in up to 2% of patients. Infection is more likely when there is a previous history of pelvic infection.
- Abortion. The operator must ensure that the patient is not pregnant.
- Intravasation of contrast medium into the venous system of the uterus
Predisposing factors to intravasation of contrast during HSG Procedure
- Direct trauma to the endometrium
- Timing of the procedure near to menstruation
- Timing of the procedure within a few days after curettage
- Tubal occlusion because of the high pressures generated within the uterine cavity
- Uterine abnormalities such as uterine tuberculosis, carcinoma and fibroids