Table of Contents
Abnormal Features seen in Plain X-Ray of the Abdomen
This will explain and analyze the abnormal conditions that can be diagnosed with Plain X-Ray of the Abdomen. The normal plain abdominal x ray findings have been described and you may want to check it before reading the abnormal findings.
Pneumoperitoneum
Free air within the peritoneal cavity is seen in bowel perforation and post operatively. Air rises to the highest part of the diaphragm on an erect film The stomach is distinguished from free air by the fact that it usually has a fluid level. It should not be mistaken for a pneumoperitoneum, which does not usually show a fluid level unless there is secondary infection (abscess). A pneumoperitoneum is seldom symmetrical and may be unilateral but usually there is a small one visible on the other side. When there is doubt on the erect film or if a perforation is strongly suspected and the film appears normal, a L lateral decubitus film is helpful. Small amounts of free air will rise to lie between the liver and the diaphragm and are more readily seen. It is important to wait for a few minutes after positioning the patient to allow any free air enough time to rise to the highest point.
The commonest cause of intestinal perforation in the tropics is typhoid fever. In the Western world, it is more likely to be either a peptic ulcer or diverticular disease. Occasionally a pneumoperitoneum may be suspected on a supine film. Collections of gas may be seen in areas where the bowel does not normally lie such as overlying the liver. Also, the outer wall of the bowel may be visible in addition to the inner wall. The double wall sign. Normally the outer bowel wall is not seen as it lies against other soft tissues of similar density.
Excessive intestinal gas
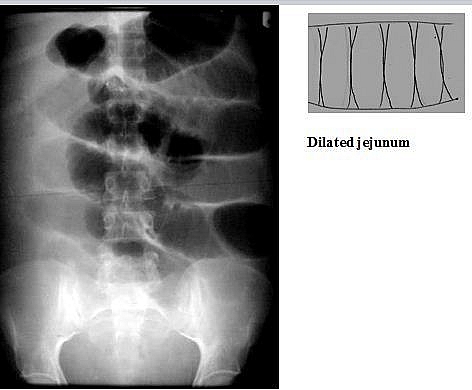
This may be physiological – children have more gas in the bowel than adults as a result of air swallowing. Patients with dyspnoea and severe pain swallow more air and if marked the bowel may be full of gas, a condition known as meteorism which is most commonly seen in renal colic. Bowel gas pattern should be evaluated with particular reference to dilatation. Excessive gas and dilatation occur in ILEUS and OBSTRUCTION. The small bowel is considered to be dilated if the width exceeds 3cm. The diameter of the colon is more variable but a width of 5.5cm is definitely abnormal.
Causes of ileus
- Post operative
- Peritonitis
- Inflammation of: Pancreas,Gallbladder,Appendix,Fallopian tubes orBowel (gastro-enteritis)
- Trauma
- Renal colic
- Ruptured aortic aneurysm
- Low serum potassium
- Drugs e.g. morphia
- General debility
- Vascular occlusion
- Uraemia
- Meningitis, malaria, or any acute severe infection
Differences between Ileus and Obstruction
- In ILEUS : both large and small bowel are usually dilated;There is more gas than fluid with few fluid levels andDecreased bowel sounds on clinical examination
- In OBSTRUCTION: Proximal bowel is dilated with collapsed distal bowel beyond the obstruction;More fluid levels and bowel diameter greater andIncreased bowel sounds on clinical examination
Fluid Levels
Fluid levels are seen when there is excess fluid and gas within the bowel. This occurs in mechanical obstruction and paralytic ileus when the bowel has ceased to function but is not mechanically obstructed. One common cause of obstruction is sigmoid volvulus. It is not always easy to distinguish obstruction from ileus and to distinguish large bowel from small bowel obstruction. Ileus may be generalised or localised.
How to differentiate large bowel obstruction from small bowel obstruction
Differentiation between large and small bowel obstruction can be difficult but things to look for are:
- Valvulae conniventesare seen in the jejunum
- Number of loops:small bowel obstruction usually shows many distended loops, large bowel obstruction few
- Distribution: small bowel lies central, large bowel peripheral
- Haustra : folds which as asymmetrical and not traversing the full width of the bowel indicate large bowel
- Diameter: large bowel has a greater width. In general if 3 – 5cms in diameter = small bowel. Over 5cm = large bowel.
- Radius of curvature. Small bowel has a smaller radius of curvature
- Solid faeces are seen only in large bowel.
Small bowel obstruction is often lower than suspected on plain films as the lower ileum may fill with fluid and become invisible. Gas will be seen at a higher level than the obstruction. The large bowel signs depend on the competency of the ileocaecal valve. If the valve is competent there is a danger of caecal perforation due to ischaemia. Critical diameter is 9cm. If the valve is incompetent, the small bowel will also dilate with excess gas and the appearances look similar to ileus. Clinically obstruction of the large bowel is more insidious in onset than that of the small bowel. Sigmoid volvulus is a common cause and shows as a dilated loop of large bowel in the shape of an inverted U with the open end pointing towards the pelvis or left iliac fossa.
In practice, it can be very difficult to differentiate ileus from obstruction and also to correctly identify the site of an obstruction on plain films.
Calcification
Abnormal intra-abdominal calcifications are common in the kidneys. Other calcifications may also occur as shown in the diagram.
- Gallstones – only 20% calcify and a plain abdomen is not indicated in cholecystitis. Ultrasound is the imaging method of choice.
- Renal tract calcification a ureteric stone is a common cause of acute abdominal pain. Many calculi are visible on plain films, especially if over 3mm in diameter. There may be bladder wall calcification in Schistosomiasis.
- Pancreatic calcification – seen in the central upper abdomen in chronic or relapsing pancreatitis.
- Adrenal calcification is less common but may be seen secondary to tuberculosis or in adrenal tumour.
- Tumours, fibroids fibroids commonly calcify and show a rather mottled appearance in the pelvis, in contrast to a bladder calculus which is laminated. Ovarian tumours rarely calcify except for dermoids, which may contain recognisable teeth.
- Calcification in the liver may occur following a successfully treated amoebic liver abscess, or in a tuberculous granuloma.
- Calcification in the spleen is rare but may follow infarction in sickle cell disease.
Gasless abdomen
Occasionally there will be a paucity of gas in the bowel on a plain abdominal film. Often this will be normal but other causes to consider are:
- High intestinal obstruction gas not passing beyond to outline the bowel lumen
- Ascites
- Excessive vomiting e.g. in severe pancreatitis
- Fluid filled bowel this may occur in small bowel obstruction and the diagnosis missed unless an erect film is taken which will show multiple very small fluid levels.
- Large abdominal mass compressing and displacing bowel
- Normal
Abnormal gas shadows
Gas lucencies lying outside the bowel lumen (excluding pneumoperitoneum). They are difficult to interpret but important diagnostically.
- Retroperitoneal gas – gas streaking in the retroperitoneal tissues along the psoas muscle and around kidneys. May be due to perforation of a part of bowel which is lying retroperitoneally (caecum, rectum) or be postoperative
- Gas in the biliary tract. This has several causes:Post operatively choledochoduodenostomy;Following passage of a large gallstone results in incompetence of the sphincter of Oddi allowing air to pass from theduodenum up the bile duct;Perforation of a duodenal ulcer into the biliary tree orAnaerobic infection especially in diabetics
- Gas in the bowel wall due to ischaemia, gangrene, and impending perforation.
- Gas in the bladder lumen vesico-colic fistula such as may occur in diverticular disease.
- Gas in the bladder wall – anaerobic infection
- Gas in the portal veins- necrotising entercolitis. Can be distinguished from gas in the biliary tree by the fact that the veins are seen extending out to the periphery of the liver whereas the bile ducts are more central.
- Abscess collections may occur anywhere. If subphrenic, they cause elevation of the diaphragm, basal lung changes, and usually show a fluid level beneath the diaphragm. Collections occurring elsewhere in the abdomen are usually missed on plain films but they may cause a mottled appearance, which looks very much like faeces in the large bowel.
Displaced bowel by masses
Hepatosplenomegaly is a common cause of abdominal mass. An enlarged spleen pushes the stomach gas shadow medially and displaces the left kidney downwards. Similarly, an enlarged liver displaces the hepatic flexure downwards. Other masses will also displace bowel and this is a clue as to their presence. Plain abdominal films are not indicated however for abdominal masses and ultrasound is the examination of choice
Abnormal bowel mucosa
This may show as thumbprinting due to bowel wall oedema or inflammation. The bowel outline shows indentations (scalloping) instead of having a smooth outline.
Fat lines
These may be displaced or lost. A bulging psoas shadow is of more significance than an absent one because they may be obscured by bowel gas and not always seen. The psoas outline is bulging or lost in rupture of an aortic aneurysm and psoas abscess.
Elevation of a diaphragm
This may be associated with changes below the diaphragm such as liver or splenic abscess. Liver tumour, ascites, or other abdominal masses, subphrenic abscess and rupture of the diaphragm.
Bony abnormality
Areas of abnormality may be seen in the spine, which may be relevant to the abdominal symptoms e.g. sclerotic areas due to prostatic metastases. There may be collapse of a vertebral body or changes in the spine or hips due to sickle cell disease.
Plain abdominal X Ray films are not always diagnostic and may be confusing. This can be enhanced by contrast medium such as inBarium Swallow, Barium Meal or Barium Enema.