Table of Contents
- Brachial Plexus Anatomy
- Formation of the Brachial plexus
- Classification of the Brachial plexus into Roots, Trunks, Divisions, Cords and Terminal Nerves
- Parts of the Brachial plexus
- The Five Roots of the Brachial Plexus
- The Three (3) Trunks of the Brachial Plexus
- The Six (6) Divisions of the Brachial Plexus
- The Three (3) Cords of the Brachial Plexus
- Peripheral Nerve Branches arising from the Cords of the Brachial Plexus
- Brachial Plexus Anatomical Variation (Prefixed and Postfixed Brachial Plexuses)
- Brachial Plexus Mnemonic
- Clinical importance and applications of the anatomy of Brachial Plexus
Brachial Plexus Anatomy
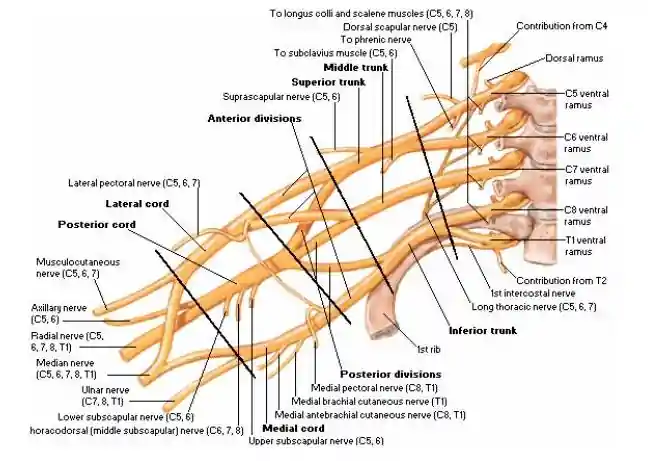
Brachial plexus is a major network of nerves that innervate or supply the upper limbs – most nerves in the upper limb arise from the brachial plexus; there is one brachial plexus on the left and another on the right, both supplying the two upper limbs. The Brachial plexus starts in the lateral cervical region (posterior triangle) and extends into the axilla where almost all branches of the brachial plexus arise after the plexus has crossed the first rib.
Formation of the Brachial plexus
The brachial plexus is formed by the union of the anterior rami of the C5 to C8 and also most of T1 nerves, which constitute the roots of brachial plexus. The roots of the brachial plexus usually pass through the gap between the anterior and middle scalene muscles to lie superior and posterior to the subclavian artery. The sympathetic fibers carried by each root of the brachial plexus are received from gray rami of the middle and inferior cervical ganglia (gray rami communicantes) as the roots pass between the scalene muscles.
Classification of the Brachial plexus into Roots, Trunks, Divisions, Cords and Terminal Nerves
The Brachial plexus is divided into different parts or segments. Starting from the origin (from the neck) to the last part as it extends into the axilla, the Brachial plexus can be divided into Roots, Trunks, Divisions and Cords.
Parts of the Brachial plexus
- There are five (5) Brachial plexus Roots
- There are 3 Brachial plexus Trunks
- There are two major Divisions of the Brachial plexus (Anterior and Posterior Divisions) of which there are 3 of the anterior divisions and 3 posterior divisions
- There are three (3) Brachial plexus Cords
Each of the parts of the Brachial plexus has nerve branches arising from it and these branches will also be mentioned briefly.
The Five Roots of the Brachial Plexus
There are five roots of the brachial plexus which are the points of origin of the brachial plexus. These roots are formed by the union of the anterior rami of the C5 to C8 and also most of T1 nerves. The roots also carry sympathetic fibers from the gray rami of the middle and lower cervical ganglia. In the lower part of the neck, the roots of the brachial plexus unite to form three trunks in this manner: the upper two roots of the brachial plexus unite to form the upper trunk, the lower two unite to form the lower trunk and the central root runs on as the middle trunk of the brachial plexus.
Branches from the Roots of the Brachial Plexus
There are three nerve branches from the roots of the brachial plexus and they are: the dorsal scapular nerve, the nerve to subclavius and the long thoracic nerve.
- The dorsal scapular nerve which supplies the rhomboid muscle arises from the posterior aspect of C5, pierces scalenus medius and courses downwards in front of levator scapulae, lying on serratus posterior superior. It is accompanied by the dorsal scapular vessels. It supplies both rhomboids and usually gives a branch to levator scapulae.
- The nerve to subclavius arises from the roots of C5 and 6 where they join to form the upper trunk. It passes down in front of the trunks and the subclavian vessels to enter the posterior surface of subclavius. It frequently has a branch (accessory phrenic nerve) which connects with the phrenic nerve, providing an alternate pathway for some fibers from the fifth cervical anterior ramus to reach the diaphragm.
- The long thoracic nerve which supplies serratus anterior arises from the posterior aspects of C5, C6 and C7. Branches of C5 and C6 enter scalenus medius, unite in the muscle and emerge from it as a single trunk to pass down into the axilla. On the surface of serratus anterior (which forms the medial wall of the axilla) this is joined by the branch from C7 which has descended in front of scalenus medius. The nerve passes down posterior to the mid-axillary line, deep to the fascia on serratus anterior, and supplies the muscle segmentally.
The Three (3) Trunks of the Brachial Plexus
In the lower part of the neck, the roots of the brachial plexus unite to form three trunks which are:
- The superior trunk formed from the union of the C5 and C6 roots.
- The middle trunk which is a continuation of the C7 root.
- The inferior trunk formed from the union of the C8 and T1 roots.
Each trunk of the brachial plexus then divides into anterior and posterior divisions as the plexus passes through the cervicoaxillary canal posterior to the clavicle.
Nerve Branch from the Trunk of the Brachial Plexus
There is only one nerve branch that arises from the trunk of the brachial plexus, this is the suprascapular nerve this nerve arises from the upper trunk in the lower part of the posterior triangle and passes backwards and laterally deep to the border of trapezius muscle. It passes through the suprascapular foramen (beneath the transverse scapular ligament) and supplies supraspinatus, and then descends lateral to the scapular spine with the suprascapular vessels and supplies infraspinatus muscle. It also innervate the shoulder and acromioclavicular joints.
The Six (6) Divisions of the Brachial Plexus
Each of the three trunks of the brachial plexus divides into an anterior and posterior division. At the outer border of the first rib, the upper two anterior divisions unite to form the lateral cord, the anterior division of the lower trunk runs on as the medial cord, while the three posterior divisions unite to form the posterior cord. There are no peripheral nerve branches arising directly from the divisions of the brachial plexus.
The Three (3) Cords of the Brachial Plexus
There are three cords (Lateral cord, Medial cord and Posterior cord)formed by the union of the six divisions of the brachial plexus. These 3 cords are related and therefore named according to the second part of the axillary artery. They enter the axilla above the first part of the axilla artery, approach and embrace the second part, and give off their branches around the third part of the axilla artery. Most of the major peripheral nerves of the upper limbs arise from the cords of the brachial plexus. Nerve branches from the lateral and medial cords generally supply the anterior compartments of the upper limbs while nerve branches from the posterior cord supply the posterior compartment of the upper limbs.
- The Lateral cord is formed the union of the anterior divisions of the upper and middle trunks and therefore has contributions from C5 to C7. It is called the lateral cord because it is positioned lateral to the second part of the axillary artery.
- The Medial cord is the continuation of the anterior division of the inferior trunk and is called the medial cord because it is positioned medial to the second part of the axillary artery. The medial cord has contributions from C8 and T1.
- The Posterior cord is formed by the union of the three posterior divisions and contains contributions from all the roots of the brachial plexus from C5 to T1. It is called the posterior cord because it is posterior to the second part of the axillary artery.
Peripheral Nerve Branches arising from the Cords of the Brachial Plexus
1. Branches from the lateral cord
There are three peripheral nerve branches arising from the lateral cord of the brachial plexus, these include the lateral pectoral nerve, musculocutaneous nerve and lateral root of the median nerve.
- The lateral pectoral nerve pierces the clavipectoral fascia to supply pectoralis major with fibers from C5, C6 and C7 and then communicates across the front of the first part of the axillary artery with the medial pectoral nerve and through this communication supplies pectoralis minor. It has no cutaneous branch.
- The musculocutaneous nerve with fibers from C5 to C7 leaves the lateral cord quite high in the axilla to run obliquely downwards and enters coracobrachialis muscle and giving a twig of supply to it before passing through the muscle. Lower down in the arm, the musculocutaneous nerve innervates biceps and brachialis and then becomes the lateral cutaneous nerve of the forearm. An anesthetic injection to the floor of the axilla in order to effect a brachial plexus block may not affect the musculocutaneous nerve because it is high in the axilla and away from the lateral cord.
- The lateral root of the median nerve is the continuation of the lateral cord (C5 to C7). It is joined by the medial root of the median nerve (from the medial cord, C8 and T1); the two roots embrace the axilla artery and when the arm is pulled down to depress the shoulder may, in some cases compress the vessel.
2. Branches from the medial cord
There are five branches from the medial cord of the brachial plexus and they are the medial pectoral nerve, medial head of the median nerve, ulnar nerve, and the two cutaneous nerves to the arm and forearm respectively.
- The medial pectoral nerve arises from the medial cord (C8, T1) behind the first part of the axillary artery and is joined by a communication from the lateral pectoral nerve. It enters the deep surface of pectoralis minor, giving a branch of supply before doing so, perforates the muscle and enters the pectoralis major, in which it ends by supplying the lower costal fibers. It may give a direct branch to pectoralis major, which passes around the lower margin of pectoralis minor. The medial pectoral nerve has no cutaneous branch. The medial and lateral pectoral nerves are named in accordance with their origins from the medial and lateral cords of the brachial plexus.
- The medial root of the median nerve is the continuation of the medial cord, with fibers from C8 and T1, and it crosses the axillary artery to join the lateral root.
- The medial cutaneous nerve of the arm (C8, T1) is the smallest and most medial of all the branches. It runs down on the medial side of the axillary vein and supplies skin over the front and medial side of the arm.
- The medial cutaneous nerve of the forearm (C8, T1) is a larger nerve that runs down between artery and vein in front of the ulnar nerve and supplies skin over the lower part of the arm and the medial side of the forearm.
- The ulnar nerve is the largest branch of the medial cord (C7, C8, T1). It runs down between artery and vein as the most posterior of the structures which run down the medial side of the flexor compartment of the arm. It sometimes receive its C7 fibers as a branch from the lateral cord, if these have not already passed to the medial cord from the anterior ramus of C7.
3. Branches from the posterior cord
The five branches from the posterior cord are the upper subscapular, thoracodorsal nerve (nerve to latissimus dorsi), lower subscapular nerve, axillary (circumflex) nerve and radial nerves.
- The upper subscapular nerve is a small nerve (C5, 6) which enters the upper part of subscapularis muscle.
- The thoracodorsal nerve (nerve to latissimus dorsi with fibers from C6 to C8) is a large nerve which runs down the posterior axillary wall, crosses the lower border of teres major and enters the deep surface of latissimus dorsi, well forward near the border of the muscle. It comes from high up behind the subscapular artery, but as it descends to enter the muscle it lies in front of the artery, at this level called the thoracodorsal artery. It is thrown into prominence in the position of lateral rotation and abduction of the humerus and is thus in danger in operations on the lower axilla.
- The lower subscapular nerve (C5, 6) is larger than the upper subscapular and supplies the lower part of the subscapularis and ends in teres major.
- The axillary nerve which is formerly called the circumflex nerve is one of the two large terminal branches of the posterior cord (the other is the radial nerve). The axillary nerve (C5, 6) supplies nothing in the axilla despite its name having been changed from circumflex to axillary nerve. From its origin, it runs backwards through the quadrangular space bounded by subscapularis above, teres major below, long head of triceps medially and the surgical neck of humerus laterally. It then passes just below the capsule of the shoulder joint, with the posterior circumflex humeral vessels below it, and emerges at the back of the axilla below teres minor. Having given a branch to the shoulder joint, it divides into anterior and posterior branches. The anterior branch winds round behind the humerus in contact with the periosteum and enters the deep surface of the deltoid muscle to supply it; a few terminal twigs pierce the muscle and reach the skin. The posterior branch supplies teres minor and deltoid, then winds around the posterior border of deltoid to become the upper lateral cutaneous nerve of the arm.
- The radial nerve (C5 to C8 and T1) is the continuation of the posterior cord, and is the largest branch of the whole plexus. It crosses the lower border of the posterior axillary wall, lying on the glistening tendon of latissimus dorsi. It passes out of sight through the triangular space below the lower border of this tendon as it lies in front of teres major, between the long head of triceps and the humerus. Before disappearing it gives nerves of supply to the long head of triceps and the medial head (a nerve which accompanies the ulnar nerve along the medial side of the arm) and a cutaneous branch which supplies the skin along the posterior surface of the arm (posterior cutaneous nerve of the arm).
Brachial Plexus Anatomical Variation (Prefixed and Postfixed Brachial Plexuses)
Variations in the brachial plexus formation are common. In addition to the five anterior rami (C5-T1) that form the roots of the plexus, small contributions may be made by the anterior rami of C4 or T2. When the superior-most root (anterior ramus) of the plexus is C4 and the inferior-most root is C8, it is called a prefixed brachial plexus. Alternatively, when the superior root is C6 and the inferior root is T2, it is a postfixed brachial plexus. In the latter type, the inferior trunk of the plexus may be compressed by the first rib, producing neurovascular symptoms in the upper limb.
Variations also may occur in the formation of trunks, divisions, and cords; in the origin and/or combination of branches; and in the relationship to the axillary artery and scalene muscles
Brachial Plexus Mnemonic
In order to easily remember the brachial plexus, it is important to appreciate the parts of the brachial plexus which are the roots between scalene muscles, trunks in the triangle, divisions behind the clavicle and cords in the axilla. The nerve branches of the brachial plexus are formed from the roots, trunks and cords; there is no peripheral nerve branch from the divisions. The roots and trunks with their nerve branches form the supraclavicular part of the brachial plexus, while the cords and their branches form the infraclavicular part of the brachial plexus.
When you learn the basic pattern, it becomes easier to put in the branches of the brachial plexus which consist of 3 branches from the roots and 3, 5 and 5 from the lateral, medial and posterior cords respectively. The only exception to the 3, 5, 5 rule is in the branch from the trunks. It is only one (the suprascapular nerve), from the upper trunk, in the posterior triangle. Everywhere else in the plexus the number of branches follows the 3, 5, 5 pattern.
Clinical importance and applications of the anatomy of Brachial Plexus
Brachial Plexus Injury
Brachial plexus Injuries affect movements and cutaneous sensations of the upper limb. Any disease, stretching or wounds in the lateral cervical region (posterior triangle of the neck) or in the axilla may give rise to brachial plexus injuries. The Signs and symptoms of brachial plexus injury depend on the part of the plexus that is affected. Injuries to the brachial plexus result paralysis (loss of muscular movement) and loss of cutaneous sensation (anesthesia). In complete paralysis, no movement is possible while in incomplete paralysis, there could be partial movements because not all muscles are paralyzed, even though the movements are weak compared to those on the uninjured side.
Brachial plexus Injuries to superior parts, affecting the C5 and C6 fibers usually occur from an excessive increase in the angle between the neck and the shoulder. These injuries can occur in a person who is thrown from a motorcycle or a horse and lands on the shoulder in a way that widely separates the neck and shoulder. When thrown, the person’s shoulder often hits a hard surface such as a tree or the ground and stops but the head and trunk continue to move. This stretches or ruptures superior parts of the brachial plexus or avulses (tears) the roots of the brachial plexus from the spinal cord. Brachial plexus injury to the superior trunk gives rise to waiter’s tip position in which the limb hangs by the side in medial rotation.
Upper brachial plexus injury can also occur in a newborn when excessive stretching of the neck occurs during delivery giving rise to Erb-Duchenne palsy due to paralysis of the muscles of the shoulder and arm supplied by C5-C6 occurs. The usual clinical appearance is an upper limb with an adducted shoulder, medially rotated arm, and extended elbow. The lateral aspect of the upper limb also experiences loss of sensation.
Prolonged micro-trauma to the superior trunk of the brachial plexus from carrying a heavy backpack can produce motor and sensory deficits in the distribution of the musculocutaneous and radial nerves.
Brachial plexus Injury to inferior parts of the brachial plexus leads to Klumpke paralysis this is less common. These injuries may occur when the upper limb is suddenly pulled superiorlyfor example, when a baby’s limb is pulled excessively during delivery. These events injure the inferior trunk of the plexus (C8 and T1) and may avulse the roots of the spinal nerves from the spinal cord. The short muscles of the hand are affected and a claw hand results.
Brachial Plexus Block
Injection of an anesthetic solution into or immediately surrounding the axillary sheath interrupts nerve impulses and produces anesthesia of the structures supplied by the branches of the cords of the brachial plexus. Combined with an occlusive tourniquet technique to retain the anesthetic agent, this procedure enables surgeons to operate on the upper limb without using a general anesthetic. The brachial plexus can be anesthetized using a number of approaches: such as interscalene, supraclavicular, and axillary approach.