Definition
Definition
Placenta previa (or Placenta Praevia) can be defined as any placenta that is either partially or wholly implanted in the lower uterine segment after 24 weeks of gestation. If the placenta lies in the anterior part of the uterus and reaches into the area covered by the bladder, it is known as a low-lying placenta (before 24 weeks). When it is still at the area covered by the bladder even after 24 weeks, it can then be referred to as Placenta Praevia.
About 5% of pregnant women will have a low-lying placenta when scanned at 16 to 20 weeks of gestation. The incidence at delivery is about 0.5%. This means 9 out of 10 women, the placenta will rise away from the cervix as the uterus grows.

Table of Contents
Classification of Placenta previa
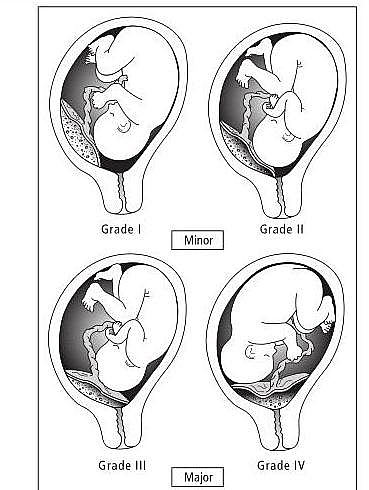
- Classical classification: Grade I, II, III and IV Placenta Praevia
- Contemporary Classification: Marginal, Lateral and Central Placenta Praevia
- Ultrasound Classification: Major and Minor Placenta Praevia
Types of Placenta Previa (Types 1, 2, 3 and 4)
- Type 1: This is also called First-degree or Placenta previa lateralis or Low-lying placenta. The placenta encroaches on the lower uterine segment but does not reach the internal os of the cervix.
- Type 2: This is also called Second-degree or Placenta previa marginalis. The placenta reaches the internal os of the cervix but does not cover it. Type IIA is also called Placenta previa marginalis anterior (the placenta is implanted anteriorly). Type IIB is also called Placenta previa marginalis posterior (the placenta is implanted posteriorly). The praevia marginalis posterior is of bad prognosis than marginalis anterior in that the posterior encroaches on the true conjugate diameter which delays the engagement of the fetal head. Engagement of the head will compress the placenta against the sacrum and cause fetal asphyxia.
- Type 3: This is also called Third-degree or Placenta previa incomplete centralis. The Placenta covers the internal os of the cervix but does not cover it completely when the cervix is fully dilated. This means the placenta covers the os asymmetrically.
- Type 4: This is also called Fourth-degree or Placenta previa complete centralis. The placenta covers the os even when it is fully dilated.

Ultrasound Classification into Major and Minor Placenta Previa
- Minor Placenta Previa: includes Type I and IIA Placenta previa
- Major Placenta Previa: This includes Type IIB, III, and IV Placenta previa
Symptoms and Signs
- Initial warning hemorrhages
- Painless vaginal bleeding that is bright red and mostly occurs following trauma, intercourse, or pelvic examination.
Causes and Risk factors of Placenta Previa
- Previous Placenta Previa
- Multiple gestations (Having twin pregnancy or more)
- Multiparity (women who have given birth several times)
- Advanced maternal age
- Uterine structural abnormality such as having Uterine Fibroid
- Assisted conception
- Diabetes mellitus
- Cigarette smoking (smoking causes carbon monoxide hypoxemia leading to hyperplacentosis)
- Previous Caesarean section: Embryos are more likely to implant on a lower segment scar from a previous cesarean section. This increases the risk of placenta accreta/increta/percreta
Placenta Previa Diagnosis
- Nowadays most low-lying placentae or Placenta previa are diagnosed by an ultrasound scan. This will show the position of the placenta clearly within the uterus.
- Presence of recurrent painless bright red vaginal bleeding
- When there is persistent mal-presentation or high head in late pregnancy
Management and Treatment
The McAfee regimen is used in Placenta previa management for pregnancies that are not up to term, in which bleeding is mild and self-limiting. The McAfee regimen is outlined below.
McAfee regimen in the management of Placenta previa
- Admit patient in a hospital facility with 24 hours services so as to monitor the patient closely
- Ensure strict bed rest in a left lateral position to improve the placental blood flow.
- Check the packed cell volume (PCV) to ensure it is not low; if it is low, give a blood transfusion to raise the PCV to 30%.
- Group and cross match 4 units of blood and ensure it is available at all times in the blood bank. This is to ensure there is blood in case of emergency (torrential bleeding or need for emergency cesarean section)
- The patient should use perineal pad which should be checked twice to monitor the volume of bleeding
- Encourage the mother to keep fetal kick chart (FKC) to monitor the fetal well being
- Regular monitoring of fetal heart rate and vital signs of the mother (Blood pressure and pulse)
- If the gestational age is less than 34 weeks, give steroids to help in lung maturation so as to be possible to deliver the fetus if the need arises such as an emergency. 12 mg dexamethasone is given intramuscularly and it is repeated again after 12 hours.
- The following back up must be readily available: Neonatal anesthesia, Caesarean section facility, and blood transfusion facility
- The following materials should also be available in case of emergency: Intranasal oxygen, 2 liters of intravenous fluid, blood giving set, wide-bore cannula (size 16 Ash color) and IV giving set
- Ultrasound should be repeated at 36 weeks
The above guidelines are referred to as the McAfee regimen. There are indications for termination of the McAfee regimen and are outlined below. Avoid all digital vaginal examinations in placenta previa; a gentle bivalve speculum examination should be performed to determine if blood is coming through the cervical os, especially if a placenta praevia has been suspected but not diagnosed definitely.
Indication for termination of McAfee Regimen
- When pregnancy has reached 38 weeks or more
- When there is Premature Rupture of Membrane (PROM)
- Antepartum Fetal distress
- Congenital anomaly
- Intrauterine Fetal Death (IUFD)
- When a patient falls into labor
Mode of Delivery in Placenta previa
- When it is Type I and Type IIA with cephalic presentation and no fetal distress, the mode of delivery is a vaginal delivery
- When it is type IIB or III or IV, the mode of delivery is Caesarean section
- If a patient presents with massive bleeding, the patient should be resuscitated and Caesarean section performed irrespective of the gestational age.
Possible Complications
- Post-partum hemorrhage (PPH) in the mother
- Puerperal infection in the mother
- Embolism in the mother
- Respiratory distress syndrome in the baby
- Preterm delivery
- Anemia in the neonate
Prognosis
The major cause of death in women with placenta previa is postpartum hemorrhage (PPH) because the lower segment of the uterus does not contract and retract as that of the upper segment. Because of this, the maternal blood vessels of the placental bed may continue to bleed after delivery leading to an emergency hysterectomy.
 Definition
Definition