Table of Contents
- Glaucoma Definition
- Glaucoma Epidemiology
- Glaucoma Risk Factors
- Glaucoma Causes
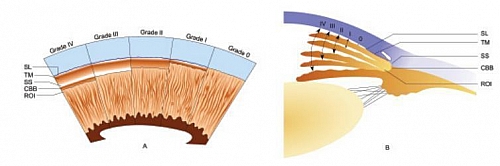
- Stages of Glaucoma: Shaffers System of Grading the Angle width in Glaucoma
- Glaucoma Classification
- Secondary Glaucoma
- Glaucoma Treatment
- Glaucoma Eye Tests (Clinical Eye Examinations for Glaucoma)
- Glaucoma Monitoring
- Glaucoma Screening
- Glaucoma Prevention
Glaucoma Definition
Glaucoma is a group of disorders of the eyes characterized by a progressive optic neuropathy resulting in a characteristic abnormal appearance of the optic disc and a specific pattern of irreversible visual field defects that are associated frequently with raised intraocular pressure. Glaucoma symptoms are mostly not evident (it is asymptomatic) and a diagnosis is made during Eye exam as described below. Glaucoma is not a single disease process but a group of different abnormalities of the eyes causing optic nerve degeneration. One may have any of the different types of Glaucoma.
Glaucoma Epidemiology
Glaucoma is the commonest of blindness that cannot be reversed in the world, this means that Glaucoma blindness cannot be reverse and once it has caused blindness, such a person becomes blind permanently. Glaucoma affects about 2% of people above 40 years of age and about 4% of elderly people above 70 years.
Glaucoma Risk Factors
Risk factors of Glaucoma include:
- Raised Intraocular Pressure (IOP) – above 20 mmHg
- Positive family history of Glaucoma
- Family history of Myopia
- Hypertension
- Diabetes Mellitus
- Long term use of steroids in the eyes
- Anemic crisis such as in sickle cell anemia
- Trauma to eyes may predispose to having glaucoma
- Cataract predisposes to developing Glaucoma
Glaucoma Causes
Causes of Glaucoma include:
- Injury or trauma to eyes
- Uveitis
- Glaucoma associated with Syndromes such as Sturge-Weber syndrome, Chandlers syndrome, and Cogan-Reese syndrome
- Rubeosis Iridis: in this, Neovascularization of the iris develops following retinal ischaemia and can be seen as a complication in sickle cell anemia, diabetes mellitus and Eales disease
- Cataract predisposes to developing Glaucoma
- Intraocular tumors or cancers
- Ciliary block glaucoma which may occur as a complication of intraocular operation or surgery
- Intraocular hemorrhage (bleeding in the eyes)
- Drug induced glaucoma such as prolong use of steroids causing Steroid-induced Glaucoma
Stages of Glaucoma: Shaffers System of Grading the Angle width in Glaucoma
There are 5 stages of glaucoma in the Shaffers system of grading glaucoma using the width of the angle between the iris and the trabecular meshwork and the structures seen on Gonioscopy. Angles of 20 degree or less shows angle closure is possible.
Glaucoma Stages
- Grade 0: 0 degree angle, and there is complete closure of angle with none of the angle structures is visible (Schwalbes line, Trabecular meshwork, Scleral spur and Ciliary body band are not seen on Gonioscopy)
- Grade 1: angle width is 10 degrees and very narrow with high chance of closure of the angle and only Schwalbes line seen on Gonioscopy.
- Grade 2: angle width of 20 degrees, moderately narrow angle with a possibility of closure and Schwalbes line and Trabecular meshwork seen on Gonisocopy
- Grade 3: angle width of 20 to 35 degrees with an open angle and no chance of angle closure with Schwalbes line, Trabecular meshwork and Scleral spur seen on Gonioscopy
- Grade 4: angle width of 35 to 45 degrees, wide open angle with no chance of closure and Schwalbes line, Trabecular meshwork, Scleral spur and Ciliary body band are seen
Glaucoma Classification
There are about 60 different types of Glaucomas that can be classified based on the age of onset, the anatomy of the eye angle, the intraocular pressure and type of causative agent.
Types of Glaucoma
- Acute Glaucoma and Chronic Glaucoma: when Glaucoma occurs within a short period of time, it is referred to as acute Glaucoma but when it occurs over a long period of time, it is said to be Chronic.
- Based on age of onset: when it occurs at birth, it is called Congenital Glaucoma and when in childhood, it is called Juvenile Glaucoma, when it occurs in adulthood, it is referred to as Adult Glaucoma.
- Normal tension Glaucoma and Ocular Hypertension: when Glaucoma occurs under normal intraocular pressure (normal intraocular pressure is 10 to 21 mmHg), it is called normal tension glaucoma but when it occurs with raised intraocular pressure without optic neuropathy, it is referred to as ocular hypertension.
- Primary Glaucoma and Secondary Glaucoma: when the causes of Glaucoma are not known, it is referred to as Primary Glaucoma and when the Glaucoma Causes are known, it is referred to as Secondary Glaucoma.
- Open Angel Glaucoma and Closed Angle Glaucoma: these are named based on the angle formed by iris and cornea. When the angle is opened on Gonioscopy, it is called open angle Glaucoma but when closed, it is called closed angle Glaucoma.
Glaucoma therefore can be named by combining two or more of the above classifications such as Primary Open Angle Glaucoma (POAG) and Acute Angle Closure Glaucoma (AACG).
Chronic primary open-angle glaucoma (POAG)
This is the commonest type of glaucoma in Afro-Caribbean and in Caucasians. It is caused by raised intraocular pressure and changes occurring in the vascular supply of the optic nerve. The risk of having Chronic Primary Open Angle Glaucoma is increased when you are of Afro-Caribbean descent, when you have a positive family history and when there is raised intraocular pressure.
Chronic primary open-angle glaucoma symptoms
Symptoms of Chronic open angle glaucoma are mostly noticed in advanced disease but remains mostly asymptomatic in the early phase. This type of glaucoma symptoms occur when there is advanced optic disc cupping and the symptoms include:
- Peripheral field defect
- Central vision is lost
- Presence of Tunnel vision
Chronic primary open-angle glaucoma signs
- Raised intraocular Pressure (IOP) of range > 21mmHg to < 40mmHg
- Normal open angle on performing a Gonioscopy
- Visual field changes such as arcuate scotoma on automated fields analysis
- Gradual thinning of the neurosensory rim superiorly and inferiorly
- Optic disc rim notching and cupping
- Nerve fiber layer defect
- Enlarged cup:disc ratio that may be assymetrical
Chronic Primary Open Angle Glaucoma Treatment
Treatment of Glaucoma includes the use of daily topical eye drops with monitoring of disc appearance and visual field analysis. Laser and surgical procedure may be done.
Acute Angle Closure Glaucoma (AACG)
This type of glaucoma is common among older age groups. It also affects people with Hypermetropia and commoner among Chinese. People having Acute Angle Closure Glaucoma may become blind when the glaucoma is neglected or undetected.
Acute Angle Closure Glaucoma Symptoms
- Sudden and severe painful red eyes
- Blurring of vision
- Presence of Halos around light
- Headache
- There may be Nausea and vomiting
Acute Angle Closure Glaucoma Signs
- Reduced visual acuity
- Red eyes
- Corneal edema (hazy cornea)
- Vertically mid dilated eyes
- Raised Intraocular Pressure (IOP)
- Closure of Iridocorneal angle on Gonioscopy, hence the name Angle Closure Glaucoma
Acute Angle Closure Glaucoma Treatment
Treatment of Acute Angle Closure Glaucoma helps to prevent permanent blindness and this involves the use of topical and systemic medications to bring lower the intraocular pressure (IOP) and break attack. Further Glaucoma attacks are prevented with YAG laser iridotomy or surgical peripheral iridectomy (in both eyes) and the second eye is treated prophylactically to prevent later Acute Angle Closure Glaucoma (AACG).
Secondary Glaucoma
Secondary Glaucoma causes include trauma to the eyes, uveitis and rubeosis iridis. The treatment of Secondary Glaucoma is to treat the underlying cause and prevent or treat intraocular pressure.
Chronic Angle Closure Glaucoma
This occurs in younger age group and may present with intermittent angle closure symptoms. This type of Glaucoma treatment is by Laser Peripheral iridotomy.
Congenital Glaucoma/Glaucoma Congenito (Infantile Glaucoma and Buphthalmos)
This type of Glaucoma occurs in babies that are less than one year of age (that is, in infants) and may occur in only one eye (Unilateral Glaucoma), but may also occur in both eyes (Bilateral Glaucoma). This type of Glaucoma is associated with ocular abnormalities and syndromes such as Sturge-Weber syndrome. A baby may go blind if this is not detected early and treated immediately.
Congenital Glaucoma symptoms include watering photophobic eyes (that is eyes that are watery and the child avoids light)
Congenital Glaucoma Signs
- Large eyes (Buphthalmos) – leading to development of short sightedness (myopia)
- Widened diameter of cornea
- Cloudiness of cornea
- Reduced vision
- Linear tears in Descemets membrane
- There may be red eyes
- Raised intraocular pressure (IOP)
Treatment of Congenital Glaucoma
Congenital Glaucoma treatment may include Goniotomy as the first choice or Trabeculotomy or Trabeculectomy.
Glaucoma Treatment
Treatment of Glaucoma is by the use of Glaucoma Medications such as beta blockers or use of Surgery such as Goniotomy,Trabeculotomy or Trabeculectomy.
Glaucoma Eye Tests (Clinical Eye Examinations for Glaucoma)
- Visual acuity Test: this is affected by advanced chronic glaucoma damage or acute angle-closure glaucoma. The Visual acuity will be reduced in any of the conditions.
- Ocular examination: Slit lamp in Glaucoma examination is use to check anterior segment abnormalities that are associated with glaucoma and also for complete assessment of optic disc. The progression of glaucoma is checked by viewing the optic disc using conventional or 3D scanning laser ophthalmoscope
- IOP measurement: the intraocular pressure is measured by using a Goldmann applanation tonometer. It assesses the force needed to flatten a defined area of cornea. This force is equivalent to the intraocular pressure. Low tension glaucoma has normal pressure range IOP, there the absence of raised intraocular pressure does not mean there is no Glaucoma.
- Visual field testing: This is done using automated perimetry to allow efficient repeat testing to detect Glaucoma progression. Classic defect detected by this method is arcuate scotoma.
- Gonioscopy: this method is used to assess the anterior chamber angle with the aid of a gonioprism lens as the anterior chamber angle cannot be viewed directly. Gonioscopy helps to check if it is open angle glaucoma or closed angle glaucoma for classification and for appropriate treament. Glaucoma diagnosis is made when a glaucomatous optic neuropathy (typical optic disc and field changes) is seen.
Glaucoma Monitoring
Once Glaucoma diagnosis is made, treatment is commenced prevent progression and continuous monitoring is required using the techniques of the glaucoma exam mentioned above.
Glaucoma Screening
Glaucoma screening is essential as most types of glaucoma are asymptomatic and remain undetected until blindness or other complications have developed of which treatment at this stage becomes helpless and cannot reverse the blindness. Glaucoma screening is important for two main categories of people are those with a positive family history of glaucoma, especially primary open angle glaucoma and also anyone above the age of 40 will have IOP measured at a sight test.
If any abnormality suggestive of glaucoma is detected during the screening, the person is referred to the hospital ophthalmology department to see an ophthalmologist.
Problems associated with glaucoma screening
Most times, you may be diagnosed of having Glaucoma but you actually do not have because of false positive results during the screening process. It is good you see an ophthalmologist to have a repeat eye test to confirm whether you truly have glaucoma or not
Glaucoma Prevention
- Proper treatment of diabetes mellitus to avoid complications such as diabetic retinopathy
- Proper care and treatment of sickle anemic patients
- Avoid long term use of topical steroids on the eyes
- Avoid causing traumato the eyes or prompt treatment of any eye injury
- Regular screening if you have family history