Table of Contents
- Type 2 Diabetes Mellitus definition
- Type 2 Diabetes Mellitus Epidemiology
- Type 2 Diabetes Mellitus Pathophysiology
- Type 2 Diabetes Mellitus Causes
- Type 2 Diabetes Mellitus Risk Factors
- Type 2 Diabetes Mellitus symptoms (High Blood Sugar Symptoms)
- Type 2 Diabetes Mellitus Diagnostic Criteria
- Oral Glucose Tolerance Test in Diabetes Mellitus
- Type 2 Diabetes Mellitus diagnosis
- Type 2 Diabetes Mellitus Differential diagnosis
- Aims of type 2 diabetes mellitus management
- Benefits of exercise in diabetes mellitus
- Type 2 Diabetes Mellitus Treatment targets
- Type 2 Diabetes Mellitus Treatment
- Type 2 Diabetic Diet Plan
- List of Drugs Used in Treatment of Type 2 Diabetes Mellitus
- Type 2 Diabetes Mellitus Prevention
- Type 2 Diabetes Mellitus Complications
Type 2 Diabetes Mellitus definition
Type 2 diabetes mellitus is a form of Diabetes Mellitus that is also known as Non-Insulin Dependent Diabetes Mellitus (NIDDM). There are different types of Diabetes Mellitus that may occur in Children, Adults and Pregnant Women. Type 2 Diabetes Mellitus results from resistance to the action of insulin on cells or it could be as a result of low or unavailable amount of insulin produced by the body. The cause of low insulin in the body can be caused by many factors (see Causes below). A diagnosis of type 2 diabetes mellitus indicates that the patient cannot utilized the blood glucose available in the body and would have to rely on drugs to help in controlling the blood glucose. A characteristic of type 2 diabetes mellitus is that there is insulin resistance.
Type 2 Diabetes Mellitus Epidemiology
Type 2 diabetes mellitus globally affects people of all races and it is relatively common in all countries affecting mostly people of increasing ages (elderly), people with obesity, and those with a Family history. In poor countries, it mostly affects the rich whereas in rich countries such as United Kingdom and United States of America, it mostly affects the Poor and reason being that it is closely associated with Obesity (The risk of having Type 2 diabetes mellitus is increased by 80 to 100 fold in people with Obesity). Sometimes, people may have Type 2 diabetes mellitus but may not be evident clinically and may remain undiagnosed for many years; most times, about 25 to 50% of this group of people comes with complications especially vascular complications when it finally becomes diagnosed. The time it takes for this group of people with clinically undiagnosed Type 2 diabetes mellitus to show signs and symptoms may be accelerated by pregnancy, some illnesses or some medications.
Type 2 Diabetes Mellitus Pathophysiology
The Pathophysiology of Type 2 Diabetes Mellitus occurs due to the following:
Insulin Resistance: the insulin produced by the body is not effective; the cells of the body do not respond to the action of insulin. This means that instead of the cells to take in glucose whenever insulin is produced, they fail to do so and so glucose accumulates in the body and becomes excess, a condition referred to as Hyperglycemia in Medicine.
Defective Insulin: in this form of type 2 diabetes mellitus, the cells are not resistant to the insulin produced but the insulin itself is defective, this abnormal insulin cannot work properly to cause the cells to absorb the glucose in the blood and this gives rise to the high glucose level in the blood (hyperglycemia).
Increased circulating level of Insulin Antagonists: this occurs when some hormones are produced in excess amounts by the body that in turn counteracts the effect of insulin in the body such as glucocorticoids.
Type 2 Diabetes Mellitus Causes
- Genetic predisposition: having a twin with Type 2 Diabetes Mellitus puts you at more than 50% risk of also having Type II Diabetes. The closer you are related by blood, the more likely you will get Type II Diabetes Mellitus. Your immediate family (Father and Mother, siblings), your first degree relative and so on.
- Low birth weight predisposes to getting Type 2 Diabetes Mellitus because poor nutrition in early life limits the development and function of beta cells(the cells responsible for production of insulin in the body that help in the reduction of blood sugar/glucose)
- Abnormal insulin action or secretion: any abnormality affecting insulin leads to abnormal function of the insulin and there would be failure to reduce the level of blood sugar (blood glucose)
Rare genetic causes of Type 2 Diabetes Mellitus
- Insulin receptor mutations characterized by Obesity, hyperandrogenism in women, marked insulin resistance and acanthosis nigricans (in which the skin becomes hyperpigmented -darkish)
- Maternally Inherited Diabetes and Deafness (MIDD): this is due to a mutation in Mitochondrial DNA. It is associated with Neuromuscular abnormalities, cardiac abnormalities and eye problems.
- Wolfram syndrome (this consist of Diabetes Insipidus, Diabetes mellitus, Optic atrophy and Deafness- DIDMOAD). This is inherited by recessively.
- Alstrom, BardetBiedl and PraderWilli syndromes associated with severe obesity and Type II Diabetes Mellitus.
- Leprechaunism, RabsonMendenhall syndrome, Pseudoacromegaly and Partial lipodystrophy: associated with severe insulin resistance
Type 2 Diabetes Mellitus Risk Factors
- Obesity
- Hypertension
- Dyslipidemias such as high levels of triglycerides, low levels of High Density Lipoproteins (HDL)
- Protein C and S deficiencies
- Microalbuminemia
- Impaired Glucose Tolerance
- Male waist circumference of more than 102cm
- Female waist circumference of 88cm
- Increased plasma uric acid
- Total cholesterol level of more than 200
These risk factors are known medically as Metabolic Syndrome.
Type 2 Diabetes Mellitus symptoms (High Blood Sugar Symptoms)
- Excessive urination (urinary frequency) (Polyuria)
- Excessive thirst to drink water: you will drink large amount of water (Polydipsia)
- Excessive hunger and eating (Polyphagia)
- Weight loss
Type 2 Diabetes Mellitus Diagnostic Criteria
According to the World Health Organization (WHO), the diagnostic criteria for Diabetes Mellitus type 2 include:
- Fasting plasma glucose of more than 7.0 mmol/L (126 mg/dL) or
- Random plasma glucose of more than 11.1 mmol/L (200 mg/dL) or
One abnormal laboratory value is diagnostic of Diabetes Mellitus in a patient with signs and symptoms or Two abnormal glucose values in patients without symptoms or signs of Diabetes Mellitus.
Oral Glucose Tolerance Test in Diabetes Mellitus
The use of Oral Glucose Tolerance Test (OGTT) is only required for borderline cases of diabetes mellitus and also for diagnosis of Gestational Diabetes Mellitus (GDM)-i.e. Diabetes occurring only in Pregnancy. This is done by first allowing the eating of unrestricted carbohydrate diet for 3 days before the test, then taking blood sample after fasting overnight and then dissolving 75g of glucose in 300ml of water for adults; or dissolving 1.75g of glucose/kg body weight in children in 300ml of water and giving it to the patient. After 2 hours (samples are taken every 30 minutes until 2 hrs and their average is taken), the blood sample is taken and the two values (fasting value and average of 2hrs after glucose) are compared.
Interpretation of Oral Glucose Tolerance Test
- If the fasting blood glucose taken shows a value of less than 7mmol/L and the 2 hr after glucose value is also less than 7.8mmol/L, then the person has no Diabetes Mellitus.
- If the fasting blood glucose taken shows a value of less than 7mmol/L but the 2 hr after glucose value is within 7.8mmol/L to 11.0mmol/L, then the person has Impaired Glucose Tolerance. Having impaired glucose tolerance places the patient at risk of future diabetes mellitus and cardiovascular diseases.
- If the fasting blood glucose taken shows a value of greater than 7mmol/L and the 2 hr after glucose value is also greater than 11.1mmol/L then the person has Diabetes Mellitus.
Type 2 Diabetes Mellitus diagnosis
The diagnosis of type II diabetes is done using Laboratory diagnosis as stated above and then using other findings such as a patient having obesity, family history, no autoantibodies detected, no Human Leucocyte Antigen (HLA) links, persistence of C-Peptide and usually occurs in people older than 30 years.
Type 2 Diabetes Mellitus Differential diagnosis
- Type 1 Diabetes Mellitus
- Diabetes Insipidus
- Thyrotoxicosis (with weight loss despite increased appetite)
Aims of type 2 diabetes mellitus management
The goals of treatment in type II diabetes mellitus includes:
- Eliminate symptoms related excess blood sugar (hyperglycemia)
- Reduce or eliminate long term complications of diabetes mellitus
- Enable the patient to live a normal lifestyle
To achieve these goals, the patient should be educated and enlightened about Diabetes mellitus.
Patient Education in Diabetes Mellitus
The patient should be Educated on the following:
- What is Diabetes Mellitus
- Nutrition and its importance in helping to manage diabetes
- Exercise and weight loss
- Foot care to avoid ulcerations
- Self-monitoring of blood glucose using tools such as Glucometers
- Good skin care
- Self-administration of Insulin
Benefits of exercise in diabetes mellitus
- Reduces cardiovascular risk of developing myocardial infarction
- Reduces blood pressure
- Maintenance of Muscle mass
- Reduction of body fat
- Weight loss
- Increases insulin sensitivity
About 150 minutes of exercise per week is good but is totally dependent on the age of the patient. Your doctor will guide you appropriately. Exercise should be avoided in those patients having Untreated Proliferative Retinopathy as vigorous exercise may lead to vitreous hemorrhage or retinal detachment.
Type 2 Diabetes Mellitus Treatment targets
When treating a patient with Diabetes Mellitus, the doctors aim to achieve certain targets that ensure good control of blood sugar level and reduce risk of developing complications. These targets are listed below.
- Fasting plasma glucose level of 4.4 to 7.2mmol/L
- Glycated Hemoglobin (HbA1c) should be less than 7%. This is what shows the doctors if a patient is complying with treatment or not. If you have been taking your drugs correctly, this will show and if you havent, it will still show.
- Blood pressure level of less than 140mmHg/90mmHg
- High Density Lipoproteins level of 1.3mmol/L for men and 1.3mmol/L for females
- Triglyceride level of 1.7mmol/L
- Weight loss of 5 to 10% after diagnosis. Losing weight will help reduce cardiovascular diseases since type 2 diabetic patients are obese.
Type 2 Diabetes Mellitus Treatment
The treatment of type 2 Diabetes Mellitus includes lifestyle modification and use of Medications that help in the control of blood glucose. The best form of treatment is to prevent it from occurring and this may be done as described below.
- Lifestyle Modifications such as daily exercise, stoppage of smoking and stopping alcohol consumption.
- Eating type 2 diabetes mellitus diet (see below)
- Use of Hypoglycemic drugs
- And use of Insulin when there is beta cell failure
Type 2 Diabetic Diet Plan
The recommended composition of type diabetes diet is described below.
- Limit the use of fat and oil in cooking, or in fried foods, processed meats (burgers, salami, sausages)
- Limit high-fat snacks such as cake, crisps, nuts, biscuits, chocolate, and pastry
- Encourage the use of lower-fat dairy products such as skimmed milk, reduced-fat cheese, low-fat yoghurt) and lean meat
- Eat fish, especially oily fish, once or twice weekly. Fish oil supplements not recommended
- Encourage use of intense artificial sweeteners instead of sugar (sugar-free fizzy drinks, squashes and cordials). Limit the use of fruit juices, cake, confectionery, and biscuits
- Sucrose: Up to 10% of total energy intake, provided this is eaten in the context of a healthy diet (examples: fibre-rich breakfast cereals, baked beans)
- Fibre: No absolute quantity recommended. Soluble fibre has beneficial effects on glycemic and lipid metabolism. Insoluble fibre has no direct effects on glycemic metabolism, but benefits satiety and gastrointestinal health
- Vitamins and antioxidants: Best taken as fruit and vegetables (five portions per day) in a mixed diet.
- Salt: should be less than 6 g per day (and should be lower in diabetic patients with hypertension)
List of Drugs Used in Treatment of Type 2 Diabetes Mellitus
- Biguanides such as Metformin
- Sulfonylureas such as Tolbutamide or Glimepiride
- Glinides such as Repaglinide
- Thiazolidinediones such as Rosiglitazone
- Alpha Glucosidase Inhibitors such as Acarbose
- Incretins such as Exenatide
- Insulin: as there is progressive beta cell failure in type 2 diabetes, the patient will eventually be placed on Insulin when the level of HbA1c is more than 8%, and in patients with high cardiovascular risk factors when HbA1c > 7%.
Type 2 Diabetes Mellitus Prevention
- Type 2 diabetes mellitus may be prevented by regular exercise
- Eating a healthy diet
- Avoid adding more weight or getting obese
- Eating food with vegetables
- Avoid drinking soft drinks having high calories or sugar
- Avoid alcohol consumption
- Avoid smoking
- Avoid sedentary lifestyle
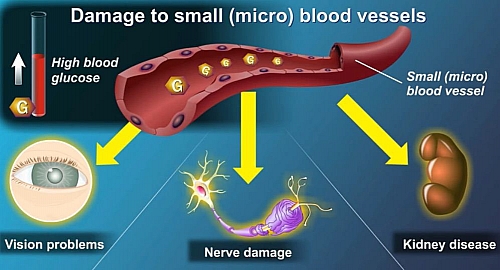
Type 2 Diabetes Mellitus Complications
- Coronary artery disease
- Peripheral vascular disease
- Stroke
- Microvascular damages such as diabetic retinopathy and nephropathy
- Neuropathy
- Lactic acidosis
- Diabetic ketoacidosis (DKA)
- Hyper Osmolar Non Ketotic (HONK) state
- Hypoglycemic Coma
- Cataract
- Impaired vision
- Myocardial infarction
- Foot gangrene leading to amputation
- Infertility
- Diabetic Foot ulcers